Lean Mass Hyper Responders After KETO-CTA: Time for a Change
Article at a Glance
- Dear Reader, I wrote this blog post last year as a follow up to my previous post titled “Why I disagree with the Feldman Lipid Energy Model.” This warning was published on the Gene Food blog out of real concern for the people adopting the LMHR protocols at the recommendation of Dave Feldman and colleagues.
- We took flack from the LMHR group on Twitter, but invited them on our YouTube channel for their perspective. They declined.
- Since this post was published, the LMHR group published a study titled KETO-CTA, which disproves the LMHR theory advanced by Dave Feldman. We now have data showing this phenotype is at heightened risk for heart disease.
- I kept most of the original blog post intact, but have overlayed with data on the KETO-CTA study in the hopes that LMHR followers will see this, and other critiques, and hopefully reconsider their protocol.
Genes Mentioned
Contents
- Update: KETO-CTA disproves LMHR theory
- Fact #3 – plaque progression was jaw dropping The subjects who started with plaque saw catastrophic progression.
- Competing theories
- The Lipid Energy Model
- Digging into a case study
- What about the sterol panels?
- LMHR Hyper Absorber?
- Dave Feldman’s response
- Challenge your assumptions
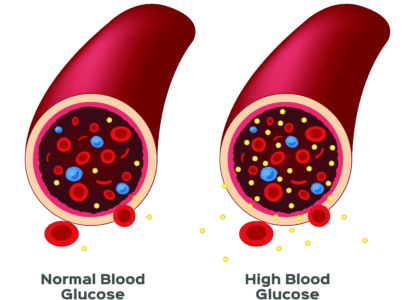
Lean Mass Hyper Responders (“LMHR”) are lean and fit individuals who see major upticks in LDL-C on low-carb and ketogenic diets. Most everyone who goes on a ketogenic diet sees some uptick in LDL-C and APOB (R), but the LMHR group reports LDL levels that would scare most cardiologists.
The LMHR phenotype is characterized by “the triad” of:
- LDL-C > 200 mg/dl
- HDL-C > 80mg/dl
- TG < 70 mg/dl
The LMHR moniker is a creation of Dave Feldman, an engineer turned lipid researcher who is skeptical high LDL levels are anything to worry about as long as the patient is insulin-sensitive.
Lipid expert Dr. Tom Dayspring first described the hyper-responder phenotype to explain cases where people see major upticks in LDL-C when following high-fat and ketogenic diets. Dr. Dayspring, whom I have interviewed twice, is adamant that even an excellent TG/HDL ratio is not protective when APOB is elevated (as it is in LMHRs).
Dave’s position paper recognizes the causal role LDL plays in heart disease in the introduction.
This dietary strategy may cause elevated LDL-cholesterol (LDL-C), an important risk factor for atherosclerotic cardiovascular disease (ASCVD)
HTTPS://DOI.ORG/10.3390/METABO12050460
This should give every LMHR pause. Notice the position paper doesn’t say “an important risk factor for atherosclerotic cardiovascular disease in patients with insulin resistance.”
I am concerned for those of you relying on the “Energy Model” as a get-out-of-jail-free card for your low-carb diets. It’s important to underscore that Dave’s position paper acknowledges the role of elevated LDL in heart disease risk. Sharing this post to the Gene Food Twitter account caused quite a stir, and several in Dave’s camp were upset with how we framed the issue. I think part of the outrage was based on the tight rope Dave walks in some of his interviews. He draws a distinction between elevated LDL based on metabolic issues, which results in high triglycerides and small dense LDL, and cases where LDL is elevated due to greater absorption or synthesis (or in his view energy expenditure).

Gerald Dropped His LDL-C by 100 Points With Diet Alone
Gerald was an ultramarathon runner, but despite his dedication to fitness, he was struggling with rising cholesterol levels, increasing blood pressure, and low energy.
It’s the latter cases where Dave seems to believe a revision of the lipid guidelines may be in order.
At the end of the day, this point is a rehash of the “large fluffy cholesterol is protective argument” that’s been kicked around for years. To be fair, Dave has said he doubts whether elevated LDL-C is dangerous when the rest of the patient’s labs are pristine. Again, he is walking a very tight rope. We can all concede that sdLDL in someone with insulin resistance is very atherogenic on a particle for particle basis due to the enhanced expression of APOC3 and increased residence time, but it doesn’t follow that “fluffy” particles are safe by contrast.
In Dave’s interview with cardiologist Dr. Ethan Weiss, at the 1:00:27 mark, he posits that LMHR may see “lower all cause mortality with higher LDL when you have the triad, I think it’s quite possible.”
To me, these types of statements are irresponsible and encourage people to continue dietary protocols that put their lipids in a bad place, and that make them unhealthier over the long term. These are the types of statements that can be reasonably interpreted as denying APOB and LDL’s casual role in heart disease, which goes against mountains of evidence. (R)(R)(R)
Since this post was originally published, Dave Feldman and colleagues published a study which destroys their own theory and proves the LMHR group is in grave danger should they forge ahead with this diet.
Update: KETO-CTA disproves LMHR theory
The new study, called Keto-CTA, by Feldman and colleagues has placed the final nail in the coffin on these arguments, yet strangely, the low carb community still insists they’re winning.
And that is why we are all in big trouble.
Things are descending into rank tribalism, fast.
The debunkers debunked themselves, but they have no plans to concede.
Dr. Tom Dayspring, and many others, have called for a retraction and censure for the peer reviewers, but the authors hail the findings as just the beginning (while launching new businesses on the back of the PR blitz).
Here are the facts surrounding Keto-CTA.
Fact #1 – lack of transparency
The “study” measured the impact of a ketogenic diet on a group of 100 LMHR over the course of one year. The authors failed to report their designated primary outcome – percent change in non-calcified plaque volume (the most dangerous, inflamed plaque).
When scientists pre-register an outcome, they make a public promise about what they’re going to measure. Skipping it after the fact undermines trust in the whole study, especially in this case because the results didn’t go the way they wanted.
The missing data? A +18.8 mm³ increase in soft plaque among those who saw progression — an alarming number for a population considered “low-risk.”
By comparison, and different cohorts have varied data, but non-calcified plaque can progress by 4–6 mm³ per year in diabetics and FH patients — not +18.8 mm³ like in the LMHR group.
The LMHR diet is a plaque factory and shows much worse results than other high risk groups.
Fact #2 – LDL-C not debunked, instead strengthened
Keto State Media on YouTube is claiming the study disproves LDL-C’s causal role in heart disease.
Boy is that dishonest.
All participants had extremely high LDL and ApoB, yet the authors conclude:
“Plaque begets plaque, ApoB does not.”
Of course baseline plaque predicts progression—but what caused the baseline plaque? The study was not equipped to answer whether lowering ApoB would prevent disease—because no participants had low ApoB to begin with. There was no control group and there can be no cause and effect if everyone has the same exposure.
This is the equivalent of:
Studying people who’ve smoked for 20 years and saying, “Lung cancer progression wasn’t predicted by cigarette use—so cigarettes must not be the problem.”
Fact #3 – plaque progression was jaw dropping
The subjects who started with plaque saw catastrophic progression.
66 participants started with zero plaque. After 1 year, plaque progressed in 6 of those 66 individuals — meaning 9% developed new visible plaque in just one year, despite being in a supposedly low risk group.
Plaque progression in this poor group of people was MUCH higher than high risk groups from other studies.
The study didn’t test whether elevated LDL-C and ApoB cause plaque—it tested whether continuing to live with already high levels predicted more plaque over just one more year.
Saying most didn’t develop plaque in year one, as the authors have, is not a defense.
Let’s contextualize with known progression rates:
In FH and diabetic cohorts:
- PARADIGM Study: Average non-calcified plaque progression ~4.7 mm³/year in mixed-risk populations
- ICONIC Study: Typical ΔNCPV = 2–6 mm³/year, even in moderate-to-high risk individuals
- ASTEROID and REVERSAL: Statin-treated CAD patients showed stable or regressed plaque over 18–24 months
In KETO-CTA:
- Those who progressed had +18.8 mm³/year, 3–5x higher than typical
- This is not typical, even for people with diabetes or FH — it suggests accelerated disease in a small but important portion of the cohort.
Competing theories
If we agree that high LDL is a risk factor heart disease, the main debate for LMHRs is why their cholesterol is high.
Dave offers the Energy Model.
The problem is that the Energy Model:
- Doesn’t respect mass balance
- Conflicts with established principles of cholesterol homeostasis, synthesis, clearance, and absorption
The Lipid Energy Model
Dave explains elevated cholesterol in the LMHR group using his Lipid Energy Model, which pins high LDL on cholesterol remnant.
Remnant cholesterol is a bi-product of the VLDL life cycle. VLDL is a type of lipoprotein that primarily traffics triglycerides and tends to be elevated in those with metabolic syndrome and type 2 diabetes.
Put simply, if your body is doing a poor job of metabolizing carbohydrates and sugars, VLDL and TG will usually be higher.
When VLDL sheds its triglyceride cargo, it re-models into a small, cholesterol-depleted particle called a remnant.
LMHR must understand remnant cholesterol
Dave believes cholesterol “ride shares” on VLDL as a type of backup energy system. According to the Energy Model, the LMHR is using so much TG for energy that the resulting remnant cholesterol causes the upticks in LDL.
The idea is that the VLDL remnant life cycle, in the aggregate, adds up to a truckload more cholesterol-rich LDL-P in the “lean mass hyper responders.”
To the uninitiated, the Lipid Energy Model is impressive, but when you look a little closer, you see it’s a house of cards.
The Energy Model doesn’t respect mass balance
As was pointed out in Dave’s interview with Peter Attia, the Lipid Energy Model doesn’t respect mass balance.
The Attia interview is crucially important because, to my knowledge, it’s the only time Dave has sat down with someone critical of his model. Most interviews he gives are with his low-carb countrymen.
Specifically, the VLDL count in the LMHR group can’t explain their elevated LDL-C because VLDL and triglycerides go down, and not up, on the diet, which makes it impossible to explain elevated LDL-C on remnant cholesterol. (R)(R)
Further, there is no good way to measure remnant cholesterol, so any claim that remnant drives elevated LDL in the LMHR cannot be disproven by any commercially available assay.
On Twitter, Dave challenges the lipid community to offer a study that shows increased cardiovascular risk in patients with an excellent TG/HDL ratio, but excludes drug and genetic studies. Why would you do such a thing when all the relevant studies are drug and gene studies?
What Dave and colleagues are really saying is, “We have to keep looking for that unicorn whose dyslipidemia is caused by remnant cholesterol even when insulin sensitive.”
In his interview on the Drive podcast, Peter Attia made the analogy to looking for someone who is six feet tall, but limiting the search to Kindergarten classes to describe Dave’s quest.
If you are staking your health on the “Energy Model,” you owe it to yourself to listen to Dave’s interview with Peter Attia and take a hard look at why Dave can’t answer the simple question – where did Moffitt get his cholesterol?
The easy explanation for the LMHR is found in the existing body of lipid science, not the Energy Model.
Digging into a case study
It’s odd Dave wants to exclude genetic and drug studies from his data sets.
For example, this LMHR case study was published by Dave and colleagues, which looks at a LMHR who went on a ketogenic diet to treat ulcerative colitis. The diet put the subject’s UC in remission but moved his LDL-C from 95 to 545 mg/dl. After 2 years, he showed a zero calcium score.
As the founder of a nutrigenomics startup, these lines from the case study were of particular interest:
Whole exome sequencing performed by Veritas Genetics, and independent dyslipidemia and ASCVD genetic risk testing by GB Healthwatch, revealed no pathogenic or likely pathogenic variants that could account for LM’s phenotype.
The LMHR in this case study was given a genetic test, and “no pathogenic or likely pathogenic” variants were found.
A quick read would have most LMHR thinking, whoa, they tested for genetics and ruled out anything hereditary as a cause of the subject’s elevated LDL. However, it’s not clear this is the case from the study because most polymorphisms that contribute to increased genetic risk for heart disease are not pathogenic; they are polygenic.
LMHR is Genetic
What if the LMHR phenotype is explained by genetics and not the Lipid Energy Model?
Pathogenic genes are defined by one gene, one condition. The analysis is binary, either you carry the marker that confers risk, or you don’t.
But that’s not how heart disease works in most cases. Genetic analysis for heart disease risk is polygenic; it doesn’t look at one or two genes. You don’t need total loss of function, as seen in most pathogenic genes, to explain significant genetic risk.
What if the search for a “pathogenic” variant in the context of the LMHR is a fool’s errand?
A review of the Supplementary Materials attached to the case study contained mostly food diaries, but not the results of the patient’s genetic testing. We do know from the case description that both the subject and his father had elevated Lp(a), which is driven by genetics, but the LPA SNPs, which must have been in the patient’s charts, weren’t listed as pathogenic.
If Lp(a), which meaningfully increases heart disease risk, and which shows up reliably in genetic charts wasn’t listed as pathogenic, what other markers were present that could have explained this individual’s dyslipidemia?
That is what we at Gene Food want to help LMHR find out.
For example, how many LMHR carry one or two copies of APOE4, a haplotype that results in a hyper-synthetic response to eating a high saturated fat diet?
Are there APOE, LDLR, APOB, PPARA, PPARG, and other SNPs that help explain risk?
We believe there likely are.

Gerald Dropped His LDL-C by 100 Points With Diet Alone
Gerald was an ultramarathon runner, but despite his dedication to fitness, he was struggling with rising cholesterol levels, increasing blood pressure, and low energy.
What about the sterol panels?
Also missing from the case study is a sterol panel, a lab test clinicians use to explain the cause of elevated lipids.
When plant sterols are elevated in the blood, it indicates increased absorption.
Conversely, when desmosterol is ticking up, it’s a sign the body is making more cholesterol.
Sterol panels defeat the Energy Model!
I suspect sterol panels aren’t included in the LMHR case studies because the results would offer a conflicting (and far more credible) explanation for elevated LDL than Dave’s “Energy Model.”
Sterol panels explain why cholesterol is elevated, which is what the Energy Model tries to do.
If an LMHR saw high levels of desmosterol alongside their sky-high LDL, it would indicate greater synthesis consistent with Dr. Dayspring’s explanation for the phenotype, not greater energy expenditure as Dave posits.
These well-established principles are at odds with the “Energy Model,” which explains upticks in LDL as caused by remnant cholesterol in insulin sensitive patients.
When confronted with a patient case study by Peter Attia named Craig Moffitt, Dave couldn’t explain why his LDL had increased using the Energy Model while also respecting mass balance.
Where did Moffitt get his cholesterol?
The LMHR is always someone who is absorbing more, clearing less, or making more cholesterol in response to dietary changes, often with clear genetic explanations. They are never seeing elevated LDL due to trafficking energy, which is not possible based on simple mass balance.
LMHR Hyper Absorber?
For example, consider this case report and accompanying study published in the Journal of Clinical Lipidology. A 13 year old presented with LDL-C of 679 mg/dl due to loss of function in the ABCG5/8 genes.
When he was placed on a low sterol and cholesterol diet, a statin and zetia, his LDL-C dropped to 60 mg/dl. This is a kid with sitosterolemia and is an extreme case.
However, in evaluating 200,000 plus subjects, the study authors found that in subjects with LDL-C >190mg/dl, 4% had sitosterol levels at the 99th percentile.
Consider that for a moment. These data demonstrate that at least a segment of the LMHR population sees very high LDL due to hyper-absorption, their high LDL has nothing to do with the Energy Model. Elevated LDL in these individuals would be explained by the very high levels of plant sterol in their blood which is a proxy marker for cholesterol absorption.
If the LMHR group uniformly dug into genetics and the results of sterol panels, each case would slowly drop away into one of three alternative explanations:
- Greater absorption (Elevated sitosterol, ABCG5/8 SNPs, Zetia)
- Greater synthesis (Elevated desmosterol, APOE, PPARA, PPARG SNPs, Statin)
- Reduced clearance (Estimated with baseline changes in absorption and synthesis, PCSK9 inhibitor)
The genes, biomarkers, and pharmaceutical interventions all line up in clear opposition to Dave’s theory.
Dave Feldman’s response
We invited Dave on the Gene Food YouTube channel to respond to this blog, but he passed. His response on Twitter is embedded below. I want to emphasize that this piece is not a personal attack on Dave; he seems sincere. However, members of our community ask us about the “Energy Model” all the time, and we wanted to have a few pieces of content to point them to, hence this post.
Ken Berry, MD, a well known advocate of low-carb diets on YouTube, also commented on this blog post on Twitter. When we asked Dr. Barry to identify alleged factual errors, he didn’t reply.
Challenge your assumptions
If you are someone struggling with these issues and looking in good faith for the reason you are seeing elevated LDL, I invite you to:
- Listen to Dave’s entire interview with Peter Attia
- Call Boston Heart Diagnostics and ask for a physician referral who runs their Cholesterol Balance Test.
- Undergo genetic testing through Gene Food or another provider to identify SNPs that can help explain your dyslipidemia. We offer a lipoprotein panel with SNPs that can explain elevated LDL, and are actively adding markers to it all the time.
When the Energy Model’s position paper acknowledges LDL’s causal role in heart disease, it seems like an unacceptable risk to walk around with these crazy high numbers just to maintain tribal affiliation.



I’ve been following Dave for a few months because I’m intrigued by the LEM (without actually understanding it) and the LMHR phenomenon, and I have grown to respect his integrity. I have no dog on this field. I don’t eat HF or keto. Dave is correct that “believes even these catastrophically high LDL levels aren’t anything to worry about as long as the patient is insulin-sensitive” is an incorrect characterization. AFAIK he has not said or implied that “belief.” He is too careful to say something like that without evidence. So maybe if you correct that statement he would engage with the details of this article? That might help ignoramuses like me learn something.
Steve, thanks for the comment. I could tell that that statement was one of the things that Dave’s camp was upset by, so I added nuance to the piece. Having said that, if you read some of his comments about the longevity potential for LMHR who fit into the triad (high LDL-C, low TG high HDL) it’s really not that far off tbh.
In Dave’s interview with cardiologist Dr. Ethan Weiss, at the 1:00:27 mark, he says that LMHR may see “lower all-cause mortality with higher LDL when you have the triad; I think it’s quite possible.”
He is walking a very tightrope.
As far as having Dave or the low-carb community engage with this content, our social media team and I had enough of just the little we saw on Twitter today. Sadly, we don’t feel a YouTube session would be productive and are no longer interested in interviewing Dave or any of his acolytes. Having said that, Dave seems like a nice dude, and I would be happy to have a beer with him (maybe a very low carb beer).