My Lp(a) is High: Here is How I Deal With It
Contents
Dear reader: the information in this post provides the basics of Lp(a) and the details of my journey after finding out their levels were elevated a few years ago. We have converted the comments section of this post to a forum where readers can share their Lp(a) stories. Discovering that you have high Lp(a) is scary and stressful, connecting with others who are in the same boat is helpful. Nothing contained in this post is medical advice. Lp(a) is a serious medical condition and requires the care of a physician. The Familial Hypercholesterolemia Foundation maintains a list of physicians who may be able to help you make sense of elevated Lp(a) numbers.
Discovering that you have elevated Lp(a) (pronounced “lipoprotein little a”) is upsetting.
I know because I’ve always had mildly elevated Lp(a).
Lp(a) production is related to inherited LPA gene variants, some of which I carry. As a result, I’ve always seen moderately elevated Lp(a) levels when I get routine blood draws.
The blog post that follows highlights some of the basics of Lp(a) research, and anticipates some of your likely questions, so you can have better conversations with your physician as you decide on a course of treatment or nutrition strategy.
First, some lipoprotein basics to set the table for the rest of the conversation.
Lp(a) under the microscope
As you can see from the chart below, the surface of LDL particles is enwrapped by a protein called apoprotein or apolipoprotein B or APOB (the gene is APOB) for short: labs and clinicians refer to it as apoB.
There is one apoB per LDL particle.
Unlike your run of the mill LDL particle, Lp(a) is a more dangerous type of apoB-containing lipoprotein. 3
Structurally Lp(a), is a cholesterol-rich, apoB-containing LDL to which a single molecule of apoprotein(a) is bound. 4
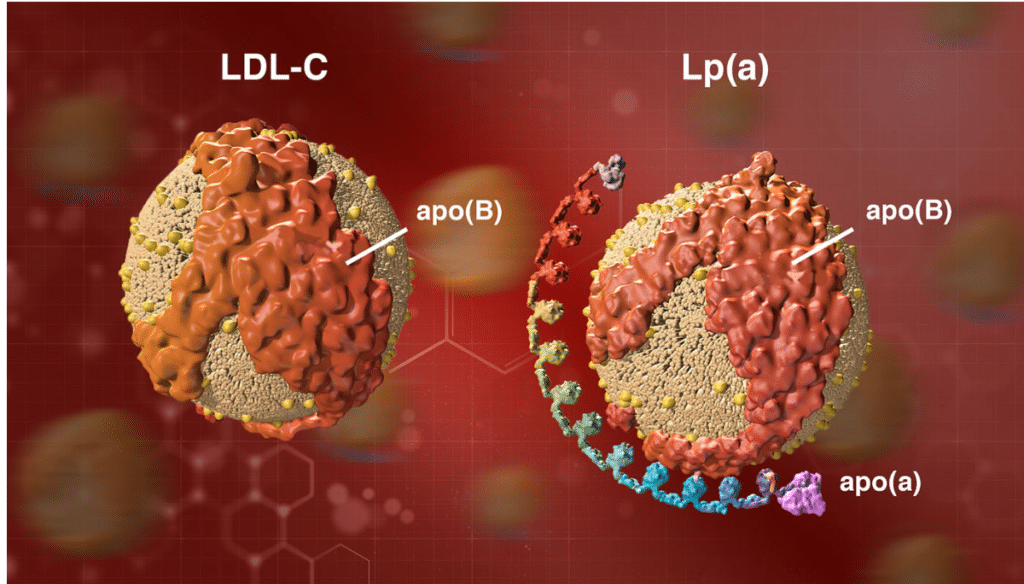
Image credit: https://www.amgenscience.com/features/10-things-to-know-about-lipoproteina/
Lp(a) testing is rare
LP(a) testing is still rare, but shouldn’t be. If you carry genetic variants that lead to high lipoprotein(a) levels, it’s important to know so you can work with a physician to treat APOB levels aggressively.
Simply doing nothing can have dire consequences.
We have seen very public examples of how elevated Lp(a) can do damage, even early in life. Celebrity trainer Bob Harper, of Biggest Loser fame, suffered a heart attack at age 52 when he appeared to be in his prime. As it turns out, the culprit was elevated Lp(a).
Although elevated levels of Lp(a) are a direct risk factor for heart disease, most “normal” lipid panels don’t even measure for Lp(a). 5
In fact, when I get Lp(a) tests done my insurance carrier often sends me a letter saying the test isn’t proven and therefore isn’t covered.
In the standard lipid panel that most of us get, Lp(a) “hides” in the LDL-C number.
What I mean here is that, absent a break out for Lp(a) specifically, Lp(a) will be included in your overall LDL-C number. 6 As the latest update in my Lp(a) numbers shows on the table below, I have had blood tests where my Lp(a) has been high despite LDL-C numbers that are fairly good at just over 100 mg/DL.
What constitutes “high” Lp(a)?
According to the National Lipid Association website, Lp(a) is considered elevated at levels greater than 50 mg/DL or 125 nmol/L.
There is strong evidence to suggest that elevated plasma Lp(a) levels (greater than 50 mg/dL or 125 nmol/L) are an independent – and possibly causal – risk factor for heart disease.
How I discovered elevated Lp(a)
Lp(a) first came on my radar after doing a Boston Heart Diagnostics Cardio panel. My lipid markers were generally ok, but at 43 mg/dl on one test, and with previous results at 46 and 49 mg/dl, my Lp(a) number was labeled “borderline.”
After reviewing my charts, my doctor told me there wasn’t much I could do to lower Lp(a).
“Lp(a) is genetic, you can’t change it all that much. It’s possible Niacin could help”
That’s never fun to hear for a metric that is tied to increased risk of heart disease, but I resolved to try nonetheless.
My Lp(a) results
While lowering Lp(a) through diet is certainly difficult, over the years, I have seen my Lp(a) number fluctuate.
Exactly why the numbers have changed is impossible to say, but I have seen rather significant changes when on different protocols.
John's Lp(a) progress
| August 2016 | |||||
| February 2017 | |||||
| November 2017 | |||||
| September 2018 | |||||
| November 2018 | |||||
| April 2019 | |||||
| June 2019 | |||||
| March 2020 |
The Cleveland Clinic references a study that looked at 5,000 patients with elevated Lp(a). When the LDL in these patients was brought down (not specified whether this was LDL-C or LDL-P), the “increased risk for mortality from Lp(a) was negligible.”
These are the studies that offer good news for those of us who need to keep an eye on Lp(a). Since Lp(a) is carried on the LDL particle, it needs LDL to do damage.
The less LDL to bind to, the less Lp(a).
This is the advice of Dr. Dayspring in the video I embedded above. High Lp(a) requires more aggressive treatment of APOB levels.
Niacin hasn’t shown real efficacy
When I first saw a blood panel that had elevated Lp(a), my doctor began discussing Niacin as a supplement, as there is some data to suggest that Niacin can reduce Lp(a) levels, although there is no evidence that Niacin reduces primary outcome clinical events in in its three major trials in persons with elevated CV-risk, and there was no event reduction even in people who saw a drop in Lp(a) when taking Niacin.
- CDP Trial – no benefit in taking Niacin
- AIM-HIGH Trial – no benefit in taking Niacin
- HPS-THRIVE Trial – no benefit in taking Niacin
The bottom line is that we have evidence that Niacin may lower Lp(a) in some individuals, but we do not have evidence it makes a difference in reducing heart attacks and strokes, and all of these trials report serious side effects in patients using Niacin.
My plan for dealing with my Lp(a)
Repatha is a PCSK9 Inhibitor that has been specifically shown to lower Lp(a) levels. I have recently switched insurance plans in favor of coverage for this drug specifically, and plan to test out my tolerance in the coming months. I would take a statin but develop bad side effects to any statin I’ve tried.
The goal here is simple, be hypervigilant about APOB levels as a risk mitigation strategy for my genetic risk with Lp(a).
Additional resources and key takeaways
For me, the key takeaway here is that elevated Lp(a) is a sign that an individual must be even more vigilant about maintaining proper “cardiovascular hygiene.” Although Lp(a) may not move with ease, it’s worth the effort to determine what drives your LDL-P number and make the changes you need to to get that number in line, which usually will mean less than 1,000.



Some studies of potential interest
https://pubmed.ncbi.nlm.nih.gov/35606076/
https://pubmed.ncbi.nlm.nih.gov/28238617/#:~:text=The%20interaction%20term%20between%20Lp,on%20the%20severity%20of%20CHD.
Get on https://www.dresselstyn.com/site/faq/
To lower LDL and total chol and for life/heart hearlth
Avoid ALL FATS GO vegan
Greens 6x a day
For LPA and valve issues PCS9-I and statins appear to be ebst
My reading seems to indicate those who take statins end up with higher LP(a).
Agreed, and true in my personal experience.
I had screening in 2018 and was found to have elevated Lp(a) and a Calcium score of 215. I was a 54 yo female at the time, father had nearly fatal MI at that age, but I had no other risk factors other than mitral valve replacement at age 38, and at that time coronary arteries were clear. 2 coronary arteries had calcifications.
Note I am a clinical pharmacist and am constantly reviewing primary studies for diet, medications, supplements and how Lp(a), LDL, CA score,and diet affect on cardiovascular risk.
I resisted statins for 1.5 years as my LDL had never been crazy high, and felt damage was likely due to Lp(a)-my opinion. I tolerated immediate release Niacin 1.5gm twice daily and my Lp(a) went from 49mg/dl down to near normal at 31, a ~36% decrease. Liver function remained normal. Adding pravastatin 10mg to Niacin increased Lp(a) to baseline of ~50, and ALT started to rise, so I stopped and stayed on Niacin alone. I was able to get LDL-C down to 98-105 on this dose, HDL rose into the 80’s. Given that “best practices” recommend LDL-c reduction to below 70mg/dl or even 55, I agreed to drop Niacin and try Rosuvastatin 5mg/day in 2019 after a secondary consultation.
Prior, I followed a mostly vegan diet for about 3.5 years from 2014-2018. I was able to decrease LDL-C, but not below 120. I have no other issues–no hypertension diabetes, obesity. I am an avid skier and moderately active the rest of the year.
Rosuvastatin 5mg alone got my LDL down to 68, though Lp(a) was also back up to 50.
Target LDL was <55, so Ezetimibe 10mg was added after 6 months. Lp(a)increased to 75. It did not have much impact on LDL and I began to have muscle pain while skiing. I stopped rosuvastatin, then tried resuming very low dose pravastatin -10mg every other day but muscle pain continued, so 1/1/21 I stopped low dose pravastatin and Ezetimibe also as well to wash out.
Two weeks later, my muscles are fine now, and I am back on Niacin 3g/day for now, as I can tolerate it. Having muscle/tendonitis issues most of my life, I have great resistance to statins as muscle problems keep me from doing what I love most.
in closing, it is very frustrating to find a path as I have known coronary artery disease without an event, and I have also found that the studies with diet below ring true as I tried going back to mediteranean diet/vegan diet, and LDL went down as Lp(a) went up.
It is also worthy to note that some of the studies that show that Niacin was not effective in reducing events were done with people already maxed out on statins, AIM HIGH, THRIVE -and the niacin was extended release combined with lapropitant–a prostaglandin D2 inhibitor to diminish flushing which ultimately was never approved. Prior to statins, Niacin did show reduction in events. I am looking into getting more detailed lab work to get the genetic profile on my lipids to guide treatment. In primary prevention its frustrating because though I appear healthy and have had no event, I have visible disease, and I am having to advocate really hard to get treatment suited to my particular genetics.
I am now adding Ginkgo Biloba 120mg daily and Red Yeast Rice 600mg daily ( low dose) as there are studies that these may lower Lp(a), and RYR has a "natural" low dose statin compound similar to lovastatin and can also lower LDL-C. Maybe my muscles can tolerate this combo, or I try adding Ezetimibe to Niacin without a statin. Time will tell.
It's hard being in the middle, and as exciting as the studies in the post below are, my Lp(a) isn't high enough to qualify for those even though I was in the 95% percentile of the calcium score for a woman my age.
For those who are reading this in late 2020 there is a clinical trial ongoing. You can check if you meet the qualification criteria below and try to enroll.
https://clinicaltrials.gov/ct2/show/NCT04023552
The world expert on lp(a) has a very educational twitter handle (below). With regards to lp(a) and diet, one could modestly reduce lp(a) at the expense of increasing LDL by going on an LCHF diet.
https://twitter.com/lpa_doc/status/1332783635330641921
The consensus view on Niacin is that it doesn’t help. But it was apparently understudied for those who have high levels and real world experience appears to show a benefit (~30% reduction) for those who can tolerate the side effects.
https://twitter.com/lpa_doc/status/1118957738661277696
With regards to lp(a) hiding out in LDL, what can be said is the following:
1. Convert lp(a) in nmol/L to mg/dl by dividing by 2.2 -2.5. e.g. 200nmol/L = 80mg/dl using a 2.5 conversion ratio.
2. The lp(a) is attached to LDL-C and the amount can be calculated using a conversion factor of ~0.3 (range 0.2-0.45). e.g. 80mg/dl lp(a) contributed 0.3*80 =24mg/dl to LDL-C
See:
https://twitter.com/lpa_doc/status/1021578377851883520
Existing treatment options include Niacin (~30% reduction) and PCSK9i (~15% reduction for those with high levels but insurance approval is unlikely). Supplementation to reduce lp(a) is not based on science. Bottom line is that there are clinical trials from Novartis and Amgen for treatments that can reduce lp(a) by ~80%. Goal for treatment for those on statins is to reduce lp(a) concentrations below 125nmol/L (and below 75nmol/l for those not on statins). On average statins raise lp(a) concentrations by ~10% though 40% of people won’t see an increase. The expected drug availability date is late 2024 assuming successful phase 3 trials and FDA approval.
I would not worry too much about Lipoprotein (a) levels since there are centenarians who also have elevated Lp(a) levels.
https://pubmed.ncbi.nlm.nih.gov/9535215/
It’s a lot more complicated than just using one blood test.
I am a 59 year old female with elevated Lp(a) 143. I was first tested about 15 years ago and it was in the low 100s(don’t remember exact count). I have been taking Crestor , niacin, and low dose aspirin, fish oil and have recently added Vit D. I recently had a Coronary Calcium test and was very disappointed to find out my score was 111 indicating moderate calcification. I have been doing a LOT of research and have been reading about Vit K2, which in combination with Vit D is suppose add calcium to bones instead of building up in arteries. The concern I have is that it also has properties to help blood clot. With Lp(a) increasing risks of blood clots , I am wondering if it could be problematic. I plan on asking my cardiologist but was wondering if anybody has any knowledge of Vit K2 and also CQ 10 impacts on Lp(a). Like many of you I am trying to be as aggressive as possible in preventing any further progression of heart disease.
I have read about the Pauling Protocol which calls for 3000 mg of Vitamin C and 3000 mg of Lysine taken daily. My Lp(a) has been 125 mg/dl. I have also been taking Vitamin D 5000 iu and methylated B. I have taken 2000 mg of Vitamin C for decades for my gums on the instruction of a dentist and snack on nuts five days a week or more. I am 52 almost 53 in a family where most of the men died very young. I also use the fish oil. When I was younger, I ate tuna and hering very often. My doctor said that I am a converter of some oil to some healthier oil. Unfortunately, I don’t understand that well. He apparently is not. It might be an advantage if I understood what he meant. I can take 40 mg of Lipitor every 2 to 3 days, and my LDL-C will be below 100. I feel like I have the flu when it gets that low in that I am shaky and my muscles are achy.
Good Info. I have come to the conclusion that cholesterol studies are a good starting point, but that you have to actually try an intervention to see if it works for you because everyone is different. What has worked for me: 1. balancing my Lipid intake, I used to consume 60% of my fat intake from Saturated fat, by replacing Butter, Heavy cream and coconut oil with Smart spreads and oils high in monounsaturated fat I lowered LDL from 180 to 135 mg/dl, do not know effect on LP(a) as I did not have LP(a) test prior to that change. I am continuing to consume a high fat diet, 65% of calories from fat. 2. Low Dose Ezetimibe, 2.5mg/day, lowered LDL from 135mg/dl to 72, LDL particle number from 1450 to 1060, APOb from 138 to 81 mg/dl, LP(a) from 90 nmol/L to 81, HDL unchanged at about 55mg/dl, Triglycerides unchanged at about 52 mg/dl. Niacin is problematic for me as even the extended release gives me bad flushes, but I am going to experiment for a month with a protocol of 500mg Niacin/81mg asprin twice a day.
Thanks John. Probably not advice most would want to follow. Seems very likely you saw decreases in lipid markers due to the Zetia and you being a hyper absorber of cholesterol.
Interesting post. Does your discussion of vegetable oils apply to olive and flax oil?
Seems it would apply especially to flax as flax is easily oxidized.
John,
It might also depend on your genetics. In spite of my lousy Lp(a), my body also apparently converts omega 6’s to omega 3’s. Apparently, not everyone is a converter. Those who are not converters apparently should avoid omega 6’s. Supposedly, my lipids improve by eating omega 6’s. I don’t fully understand what I should be doing.
I have read about the Pauling Protocol which calls for 3000 mg of Vitamin C and 3000 mg of Lysine taken daily. My Lp(a) has been 125 mg/dl. I have also been taking Vitamin D 5000 iu and methylated B. I have taken 2000 mg of Vitamin C for decades for my gums on the instruction of a dentist and snack on nuts five days a week or more. I am 52 almost 53 in a family where most of the men died very young. I also use the fish oil. When I was younger, I ate tuna and hering very often. My doctor said that I am a converter of some oil to some healthier oil. Unfortunately, I don’t understand that well. He apparently is not. It might be an advantage if I understood what he meant. I can take 40 mg of Lipitor every 2 to 3 days, and my LDL-C will be below 100. I feel like I have the flu when it gets that low in that I am shaky and my muscles are achy.
I see a clinical lipidologist at UCSF in 2 weeks. Curious what can be some to help my numbers. 45 years old. 5’4” 130#
TC 302
HDL 60 😇
Trg 134
LDL 213
LP(a) 287 nmol/L
Statins and I have never been friends.
Heidi, thanks for the comment. Most lipid experts agree that statins save lives, but clearly some people do have side effects.
Hi John,
I am considering starting Vit K 2 to help reduce calcification in my arteries and hopefully go to my bones since I have osteopenia. My concern is that Vit K2 promotes blood clotting. Do you have any info on its safety in correlation to elevated Lp(a)?
Hi Donna, this is definitely a question for your cardiologist. I don’t have any info on Vitamin K2 specifically with Lp(a), I know it’s a nutrient some cardiologists like Dr. Kahn like, but I haven’t heard it discussed in the context of Lp(a).
What protocol was suggested? Has it been effective?
I’m an active 55 year old female. 5’6 120 pounds. My father died of heart attack/stroke at 45. I have these results.
HDL 95
Triglyceride 67
LDL 99
LPA 129.
Due to family history I am quite freaked out by the LPA, Doctor had wanted to put me on a statin but I’m afraid of side effects and now it seems a statin does not even work for the LPA? I’m confused and freaked out. Please advise.
sorry that is 129 mg/dl, not nmol.
Stella, this is a question for a physician. I recently had the opportunity to interview two excellent physicians on this topic: Dr. Joel Kahn and Tom Dayspring. Adding the links to the interviews here: https://www.mygenefood.com/podcast/34-dont-ignore-high-ldl-tg-hdl-ratio-lpa-cholesterol-absorption-and-more-with-tom-dayspring-m-d/
https://www.mygenefood.com/podcast/26-lpa-the-hearts-silent-killer-with-dr-joel-kahn-m-d/
Just received my lp(a) labs today after seeing my LDL-C incrementally go up over the past few years from 100 to 127 (although two weeks after the initial tests, now 120??). Anyway, the following are my latest numbers and general info:
38 yo male; 160 lb, 5’7″, non-smoker, decent diet at the moment could be better but not horrid; exercise moderately (cardio machines, tennis, hike with dogs etc.). Overall fairly healthy
lp(a): 402 nmol/l
LDL-P: 1414 nmol/l
LDL-C: 120 mg/dl
HDL-C: 43 mg/dl
HDL-P: 25.1 umol/l
TG: 115 mg/dl – up from 100 2 weeks ago
TC: 186 mg/dl – down from 195 2 weeks ago
From talking briefly to my primary physician who prescribed a low dose of statins (haven’t taken any yet), and reading on the internet, it is apparent that my lp(a) numbers are insanely high, the LDL-C and LDL-P are in the borderline higher range and the HDL values could be a bit higher. As far as I am aware there isn’t any family history of heart issues other than my great grandfather had a heart attack, but he smoked like a chimney. My dad is taking prazastatin sodium, but his numbers are good for the most part; unsure of his lp(a), however.
It seems that is is worth making significant modifications to my diet and see what that does. Do you guys have any other thoughts, recommendations? Is being on a statin regimen worthwhile? I am planning on seeing a cardiologist in the near future to get more input. . This is a little overwhelming at the moment.Thanks for any insight.
Hey Eric, thanks for the comment. The statin question is definitely one for your doctor. Most of the top level lipid experts seem to overwhelmingly that statins are helpful and that they can make a meaningful difference in preventing heart disease. I had the chance to interview Dr. Tom Dayspring recently and we got into a number of these issues: https://www.mygenefood.com/podcast/34-dont-ignore-high-ldl-tg-hdl-ratio-lpa-cholesterol-absorption-and-more-with-tom-dayspring-m-d/
My doctor says I’m an enigma..
The ratios all look very good
TC/HDL = 3.3 (300/90)
TG/HDL = 0.67 (60/90)
ApoB/ApoA1 = 0.62 (123/197)
But there’s heart disease history in the family.. so he wants to use a statin (Atorvastatin) to see if he can lower the Lp(a) of 88 nmol/L and TC of 300.
Any thoughts if I should first check to see the % blockage using the Coronary Calcium Score and/or a carotid ultrasound?
Hey Ben, this one is definitely a question for your doctor.
John excellent article,
I was diagnosed with extensive blockages on all 3 arteries and ended up having stents – June 2018.. My Lipid panel always had been within range(upper level). I’m in good physical condition, regularly exercise and age 47. Since the stents I’ve been put on a high dose of statins. Last December I was checked for LPa and found to have very high level at 175 nmol/L. I have been on a strict vegan diet since August/2018. I did my blood work a week ago and found to have LPa at 767mg/L ( 191 nmol/L). Rest of my lipid panel is ultra low: Cholesterol 1.4 mmol/l; LDL 0.5mmol/l; HDL 0.71mmol/l; non HDL 0.7mmol/l; Risk Ratio 1.99; Triglycerides 0.45 mmol/l; Just like you mentioned I was very optimistic of being a vegan but now at a loss with these results. Very much appreciate any thoughts.
I would try having the sterol discussion with your doc and seeing what he / she says.
John
Thanks John. I strictly follow Esselstyn diet, so technically I shouldn’t have high levels of Steriols. My HbA1c is 5.7%. My GP is not aware of checking steroils in blood work so will have to wait until I see my cardiologist in 2 months. I have not been taking any fish oil as Esselstyn diet don’t recommend any of that. I’m in doubt whether I should take any. Also another interesting point – I’ve been referred by a Cardiologist from South Asia stating that a herbal supplement consisting of 3 plant ingredients(named Thripala consisting of “Aralu, Bulu and Nelli”) known to reduce LPa in South Asians. I’ve been taking it for the last 2 months but there is no visible change in LPa. Wish I could get to the bottom of this.
Thanks again!
Thanks to all,
More information than I have been able to find anywhere else on LP(a) issues. I am a 61 year old very healthy woman. After reading Peter Attia’s articles and podcasts, I decided to test my LPa (against my primary care physician’s judgement). I was shocked to see an LPa level of 255nmol/l ! Yikes!!!!!! My Triglycerdies have always been low 42, HDL 73, calculated LDL 91. My glucose is low IGF1 low and have never had any health issues. I exercise a few hours a day and eat healthy. Haven’t tried any special diets for any extended period. I’m having a Coronary Calcium Test Thurs.
I have read in some studies that even if your LPa is high, as long as your Trigycerides are low, it shouldn’t be a coronary risk but none of us want to take that gamble. Like the rest of you I am scrambling to try and figure out something I can do to avoid a cardiac event.
I will keep reading here and really appreciate all the information. Thx!
Hi Lin, thanks for the comment. I haven’t read anything indicating that low TG protect against high Lp(a).
Do check your liver enzymes when taking daily niacin. Once daily Rugby brand extended release 500mg/day niacin lowered my high Lp(a) by about 15%, so my doc said to take it twice a day. I decided to check my liver enzymes because I’d read that niacin can negatively affect them. My liver enzyme markers for inflammation were high enough that my doc said to go back to niacin once per day. In the meantime, 500mg of citrus bergamot (Jarrow) daily lowered my high LDL by 50 points, so I recently started taking it twice daily. Has anyone tried that? Next I’m adding in berberine for further cholesterol control. Has anyone had good results from that? Thanks John and everyone!