My Lp(a) is High: Here is How I Deal With It
Contents
Dear reader: the information in this post provides the basics of Lp(a) and the details of my journey after finding out their levels were elevated a few years ago. We have converted the comments section of this post to a forum where readers can share their Lp(a) stories. Discovering that you have high Lp(a) is scary and stressful, connecting with others who are in the same boat is helpful. Nothing contained in this post is medical advice. Lp(a) is a serious medical condition and requires the care of a physician. The Familial Hypercholesterolemia Foundation maintains a list of physicians who may be able to help you make sense of elevated Lp(a) numbers.
Discovering that you have elevated Lp(a) (pronounced “lipoprotein little a”) is upsetting.
I know because I’ve always had mildly elevated Lp(a).
Lp(a) production is related to inherited LPA gene variants, some of which I carry. As a result, I’ve always seen moderately elevated Lp(a) levels when I get routine blood draws.
The blog post that follows highlights some of the basics of Lp(a) research, and anticipates some of your likely questions, so you can have better conversations with your physician as you decide on a course of treatment or nutrition strategy.
First, some lipoprotein basics to set the table for the rest of the conversation.
Lp(a) under the microscope
As you can see from the chart below, the surface of LDL particles is enwrapped by a protein called apoprotein or apolipoprotein B or APOB (the gene is APOB) for short: labs and clinicians refer to it as apoB.
There is one apoB per LDL particle.
Unlike your run of the mill LDL particle, Lp(a) is a more dangerous type of apoB-containing lipoprotein. 3
Structurally Lp(a), is a cholesterol-rich, apoB-containing LDL to which a single molecule of apoprotein(a) is bound. 4
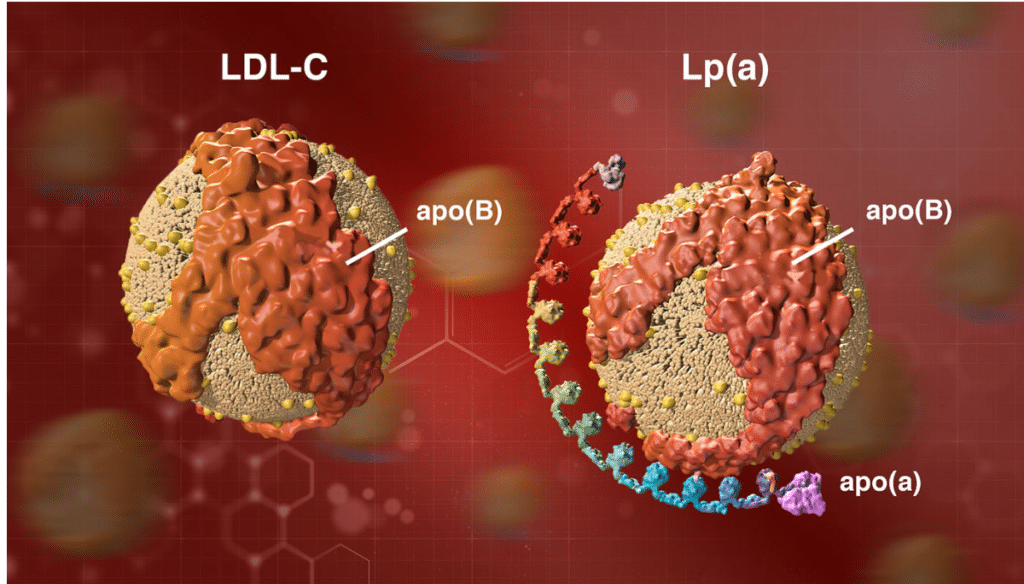
Image credit: https://www.amgenscience.com/features/10-things-to-know-about-lipoproteina/
Lp(a) testing is rare
LP(a) testing is still rare, but shouldn’t be. If you carry genetic variants that lead to high lipoprotein(a) levels, it’s important to know so you can work with a physician to treat APOB levels aggressively.
Simply doing nothing can have dire consequences.
We have seen very public examples of how elevated Lp(a) can do damage, even early in life. Celebrity trainer Bob Harper, of Biggest Loser fame, suffered a heart attack at age 52 when he appeared to be in his prime. As it turns out, the culprit was elevated Lp(a).
Although elevated levels of Lp(a) are a direct risk factor for heart disease, most “normal” lipid panels don’t even measure for Lp(a). 5
In fact, when I get Lp(a) tests done my insurance carrier often sends me a letter saying the test isn’t proven and therefore isn’t covered.
In the standard lipid panel that most of us get, Lp(a) “hides” in the LDL-C number.
What I mean here is that, absent a break out for Lp(a) specifically, Lp(a) will be included in your overall LDL-C number. 6 As the latest update in my Lp(a) numbers shows on the table below, I have had blood tests where my Lp(a) has been high despite LDL-C numbers that are fairly good at just over 100 mg/DL.
What constitutes “high” Lp(a)?
According to the National Lipid Association website, Lp(a) is considered elevated at levels greater than 50 mg/DL or 125 nmol/L.
There is strong evidence to suggest that elevated plasma Lp(a) levels (greater than 50 mg/dL or 125 nmol/L) are an independent – and possibly causal – risk factor for heart disease.
How I discovered elevated Lp(a)
Lp(a) first came on my radar after doing a Boston Heart Diagnostics Cardio panel. My lipid markers were generally ok, but at 43 mg/dl on one test, and with previous results at 46 and 49 mg/dl, my Lp(a) number was labeled “borderline.”
After reviewing my charts, my doctor told me there wasn’t much I could do to lower Lp(a).
“Lp(a) is genetic, you can’t change it all that much. It’s possible Niacin could help”
That’s never fun to hear for a metric that is tied to increased risk of heart disease, but I resolved to try nonetheless.
My Lp(a) results
While lowering Lp(a) through diet is certainly difficult, over the years, I have seen my Lp(a) number fluctuate.
Exactly why the numbers have changed is impossible to say, but I have seen rather significant changes when on different protocols.
John's Lp(a) progress
| August 2016 | |||||
| February 2017 | |||||
| November 2017 | |||||
| September 2018 | |||||
| November 2018 | |||||
| April 2019 | |||||
| June 2019 | |||||
| March 2020 |
The Cleveland Clinic references a study that looked at 5,000 patients with elevated Lp(a). When the LDL in these patients was brought down (not specified whether this was LDL-C or LDL-P), the “increased risk for mortality from Lp(a) was negligible.”
These are the studies that offer good news for those of us who need to keep an eye on Lp(a). Since Lp(a) is carried on the LDL particle, it needs LDL to do damage.
The less LDL to bind to, the less Lp(a).
This is the advice of Dr. Dayspring in the video I embedded above. High Lp(a) requires more aggressive treatment of APOB levels.
Niacin hasn’t shown real efficacy
When I first saw a blood panel that had elevated Lp(a), my doctor began discussing Niacin as a supplement, as there is some data to suggest that Niacin can reduce Lp(a) levels, although there is no evidence that Niacin reduces primary outcome clinical events in in its three major trials in persons with elevated CV-risk, and there was no event reduction even in people who saw a drop in Lp(a) when taking Niacin.
- CDP Trial – no benefit in taking Niacin
- AIM-HIGH Trial – no benefit in taking Niacin
- HPS-THRIVE Trial – no benefit in taking Niacin
The bottom line is that we have evidence that Niacin may lower Lp(a) in some individuals, but we do not have evidence it makes a difference in reducing heart attacks and strokes, and all of these trials report serious side effects in patients using Niacin.
My plan for dealing with my Lp(a)
Repatha is a PCSK9 Inhibitor that has been specifically shown to lower Lp(a) levels. I have recently switched insurance plans in favor of coverage for this drug specifically, and plan to test out my tolerance in the coming months. I would take a statin but develop bad side effects to any statin I’ve tried.
The goal here is simple, be hypervigilant about APOB levels as a risk mitigation strategy for my genetic risk with Lp(a).
Additional resources and key takeaways
For me, the key takeaway here is that elevated Lp(a) is a sign that an individual must be even more vigilant about maintaining proper “cardiovascular hygiene.” Although Lp(a) may not move with ease, it’s worth the effort to determine what drives your LDL-P number and make the changes you need to to get that number in line, which usually will mean less than 1,000.



So today I look at my labs drawn in July and December. The first time my Lp(a)-P was 745. December, it is 750. My HDL-C is 117. I am not overweight. I don’t get to exercise. I am under a lot of stress due to family situations. I’m a 58 y/o female. Comments, anyone? Am I in serious danger? I have already had heart surgery due to a birth defect, discovered when I was 52. Bad, bad genes.
hello all. i am a 38 year old female. i’m 5’9”, 160 lbs and do 30 minutes of exercise 5 days per week on my elliptical. i recently had my Lp(a) tested and it came back high, along with my lipid panel. my two different Lp(a) test numbers were as follows:
Lp(a)- 57mg/dl
Lp(a)-110 nmol/L
LDL- 128
TOTAL CHOLESTEROL- 202
My cardiologist wanted to put me on a statin, but i declined. instead i adopted a whole foods plant based diet, with no oil and no wheat. i eat only whole grains, legumes, vegetables and fruit and lots of leafy greens. i’d say my carb intake is high with all the brown rice, oatmeal and potatoes. 4 months later and my new lipid panel numbers are as follows:
LDL- 64
TOTAL CHOLESTEROL- 122
i wanted to pass along this info with my lipids and my diet incase it was helpful to anyone. i’m also looking to get any pointers on how to lower my Lp(a). i have been told that if one reduces LDL cholesterol, it renders the Lp(a) harmless. is this accurate, or do i need to be seeking out other remedies to lower this Lp(a) still? thank you all so much, glad to be connected here.
Thanks for the comment Lucy. What happened with your Lp(a) on the Whole Foods, plant based diet?
oops, i left that part out. in nmol/L, my Lp(a) has gone from 103 down to 88, then 82, then up to 110. i have not re-tested in mg/dl yet. i’m really not sure which is more accurate either. my cardiologist told me not to waste time worrying about Lp(a) any longer since my LDL is so low at 64. but of course, i like to do my own research and learn from others who have this condition.
Hi June, thanks for the comment. This is a situation for your physician to handle, they will be able to order tests that will help gauge risk.
Would digestive enzymes work as well to breakdown the fat?
Hi, Thanks for all the info. I had my LP(a) tested for the first time and it’s a terrifying 215. My CRP score is 10.3 as well. I work out (strenuously!) take fish oil, and eat mostly low carb with good fats. My Good cholesterol has always been a bit high throwing off the total cholesterol but recently my LDL got up to 147 and triglycerides are 85. I’m trying to determine what diet to follow as I’ve gotten conflicting advice. I’ve just added sublingual B12 and niacin. Do you have any suggestions for supplements,diet, and even pharmaceuticals? at this point I’m pretty nervous. Thanks!
Like you, John, I got dramatic 33% lower results when I changed to vegan. My Lp(a) dropped from 90 to 68 to 59 over 11 months, as measured by the Boston Heart Test. … For 20 years, doctors denied that my chest pains indicated a heart problem because I was so fit & all tests were good. Finally one ordered the Calcium CT scan: a whopping 327: CVD. (Personally I attribute it to the tablespoon of saturated coconut oil I’d added to my oatmeal for 2 years at the recommendation of ill-informed friends.) Good, knowledgable doctors, including cardiologists, are v. hard to find.
I did Dr. Dean Ornish’s 9-week “Reversing Heart Disease” program, which is covered by Medicare & many insurance companies (because it works). It takes some discipline. No meat, fish or dairy (I do non- fat cottage cheese & yogurt, tho, to stay above 90 lbs.! .. Weight melts away.) Also limited to a max. of only 10 grams of fat/oil/day. A smart cardiologist put me on time-released Niacin (no side effects).
On the basis of my own research, largely from Life Extension, I also take lysine-proline, algae-based Omega-3 + DHA, Alcar & Turmeric. (Will bring back the Vit. C I’d been taking now after reading your posts here.) A nurse told me she’d seen positive results reversing plaque with 360 mg. of Vitamin K2-7per day. Supposedly takes almost a year before you want to re-test your
Cal CT score.
Wow, thanks for sharing Cathy, very inspiring. Curious, what did your sitoserol levels look like on the Boston Heart panel? One of the issues that has come on my radar recently has been the interplay between oxidized phospholipids and the atherogenic nature of LP(a). Seems that oxidized phytosterols preferentially bind to Lp(a). As such, I avoid plant based omega 3 supplements because they are so high in sterol…
I read the article but don’t fully understand the whole plant based omega 3 thing?? What do you take instead
Xavier, not sure I follow, can you rephrase?
What about using Lipase enzymes? Couldn’t that be effective in breaking it down? I just had my genetic testing done and out of the 27 snps I am +/+ for 24 of them. Big wake up to the LPL. Overwhelmed in how to approach this, but you have given a start and things to look into. Thank you!
Thanks for this article and comments!
Yes, LP(a) can be reduced with Linus Pauling protocol!
My total cholesterol has been consistently high 294, with HDL of 103, LDL 178, triglycerides 64. I eat low carb and exercise. After reading Dr Linus Pauling’s research, I had my LP(a) tested and it was 55 nmol/l which is below the 75 nmol/l limit-but I wanted to see if I could lower it. My Dr kept insisting that my high total cholesterol was genetic and must be reduced with statins. I agreed with the genetics, not the statin therapy. I started on the Pauling protocol, 2000 mg Vit C, 1000 mg L-Lysine, 1000 mg proline 3 times per day…no side effects. After 4 months my LP(a) test is now 38 nmol/l! I intend to test to ascertain if this regimen has impacted my cholesterol scores in the near future.
I’d like to join these discussions. I’ve been working on my own N=1 for nearly 18 years now. I’ve got high Lp(a) and have worked with the Philadelphia Heart Institute (PHI) and other lipid researchers for nearly two decades. My diet has been my own modifications.
I did my own research when the PHI recommended a different diet (AHA diet – too high in O-6 fats). My Lp(a) was 165 ng/ml at that time. I had an EBCT scan to look for calcification and the scan found nothing. I’ve had to research and figure out my own diet, but now I’m wondering, like John, if it’s time to consider a vegetarian diet. I’m happy to share my numbers, comments from my cardiologist (a research lipidemiologist from MUSC) about diet, and my own anecdotal evidence. And I’m looking for motivation to experiment once again with diet.
For information — I achieved my best numbers against all predictions from the PHI at age 65 when my TC reached 197 and my Lp(a) reached 14 ng/ml. My diet consisted of an egg in the morning, some sauteed greens like spinach (coconut oil) mid morning, 3 – 4 ounces of salmon around noon, and a salad with olive oil by 2pm. I was using Intermittent fasting without knowing it back then. But I also was walking 7 or 8 miles 3 or 4 times a week, lots of hills (felt like HIT), and I lost a lot of weight. Carbs minimal. No grains, no processed foods, and no bad oils. I supplemented with high doses of D3 and K2.
I don’t know where to begin. At this point, my status is that I do not have any calcification according to a recent EBCT scan (age 71), do not have any cardiac symptoms (considered asymptomatic Lp(a)), take 2G of niacin ER daily, have very good blood work all around, according to my cardiologist (excellent IR, HbA1c, LDL particle size, HDL).
But I’m interested in experimenting with less animal saturated fats, more veggies, and some supplements. I’ve seen the research on saturated fats regarding how they lower Lp(a), but wondered whether this is animal or vegetable saturated fats. I cannot get enough Omega-3 from wild caught Pacific salmon and my cardio doc suggested supplements for this. I just started these. She herself takes those herself in the form of Carlson’s fish oil.
So I hope this is a viable form and I can learn more. ~~ Thanks, Cindy
Cindy, thank you so much for the thoughtful comment, quite interesting. In particular, the research on saturated fat you mention is definitely food for thought, although if you have to sacrifice high TC for high Lp(a), maybe not worth the switch? Did you have your LDL-P measured through this process? Please keep us updated with your progress.
John
Thanks for the reply, John. I did have the LDL-P measured and my numbers are really low risk, according to my cardiologist – in the lowest category. She is really surprised by the low LDL-P and even IR. As it turns out, when I drop my Lp(a), my TC also drops as do both LDL and Trigs. My highest TC occurred when I was vegetarian, but I think that is because I relied on grains (and some bread) and beans for the main portions of the meal. Since then, I sprout my beans before cooking and avoid breads and grains.
I’m really curious as to whether you’ve had good luck with lowering Lp(a) by eating whole grains. This is still a gray area for me. Also, do you think the saturated fats from a food like avocado works to keep the Lp(a) down? Currently, I try to balance out any saturated fats I eat each day, try to keep quantities down, including nuts.
But I think there are other factors to the elevated Lp(a). I cut calories and dropped about 15 lb, as well as lowered the HbA1c from 5.7 to 4.9. I walked 35-40 miles per week on hills. I believe that my pretty much avoiding mammal saturated fat except for salmon and halibut from Alaska (3-4 oz 4 or 5 times a week) and the daily egg may have had something to do with these better numbers. And I started taking the Niacin and D3 with K2 (10,000 IU of D3). I don’t think this is a monolithic process.
The doctor at PHI also thought that my inclusion of red wine 4 or 5 times a week contributed to the lower Lp(a). I know drinking alcohol is controversial over all, but I suspect that a strong exercise program and healthy weight might keep the alcohol from doing a lot of damage. So much about genetics here, I guess.
Now I’m trying to figure out the next stages with Lp(a). If I do not take my 2G of Niacin ER daily, my TC will begin to creep up as will the LDL and Lp(a). But I’ve never had a reading as high since the original reading of 165 ng/ml. Since age 65 when I did that turnaround, my highest Lp(a) reading has been about 20.
Are you exploring any dietary changes?
Thanks, Cindy
What Niacin brand are you taking and do you split it up at all.. I have very high LDL
Hi Cindy! Love reading your post. Congrats on your progress. Can you share who you work with at PHI if you are able? We are at the beginning of our journey with my husband and we live in the Philly area and I’d like him to see a specialist and get a scan as a start.
I have been conducting my own self testing and you may find it interesting and counter-intuitive but please take it seriously. I had a reasonable Lp(a) in the 30’s then I went on a low carb diet and it dropped to below 10. My research indicates it is the combination of carbs and fats that lead to high Lp(a). In other words you can eat butter and meat by themselves but you can’t eat butter on a potato. I suspect french fries are as dangerous as cigarettes. Genetics, however, are probably the overwhelmingly defining factor.
Thanks for the comment Ricky. When I went low carb, I saw a modest reduction in Lp(a), but it wasn’t until I targeted LDL-C that I saw a meaningful reduction. What was your LDL-C and LDL-P on the different diets?
John,
Great article- super helpful to me as I am 27 yo and have had a high Lpa level since I can remember! I had two questions though.
1. Does taking ghee in coffee via bulletproof coffee formula, would that be bad for someone who has a high Lpa? I know they say ghee doesn’t elevate LDL but for someone who has high levels borderline even on medication, I don’t want to mess around but I want the benefits that bulletproof coffee has to offer!
2. Would you want to take bergamot at the same time as that medication listed?
-robin
Hi Robin,
I can’t speak to your situation, but can say that for me, ghee and butter is a no go when I am focused on reducing Lp(a). What has worked for me is diet that is largely plant based. Based on the research that is out there, Niacin and fish oil seem like supplements worth experimenting with, but be sure to discuss with your doctor first. Good luck!
What supplements are best to lower LDL-P and LP(a)? Would taking 1000 mg Niacin per day be good and does it cause liver damage and insulin resistance?
The latest research hasn’t found any benefit from taking Niacin.
I am 63 and just got tested (Acessa Labs) for Lpa and Lpb and cholesterol particle size once I learned I have the LPA gene via 23&Me genetic testing. I have had high LDL for years (genetic from my mom) but my cardiologist said no need for statins since I am vegetarian (38 yrs), walk briskly 5 hrs per week, and my heart scan shows I have zero calcium plaque. BUT, since last year my LDL has gone up from 260 to 310 (LDL 225/ HDL 57). As feared, my Lpa is quite high at 175 nmol/L and Lpb is high at 144 mg/dl. Small cholesterol particle size is normal, large is slightly low, but medium size is very high at 584 nmol/L. I saw no results on cholesterol P. I take T3 and T4 for mild hypothyroidism. Other than losing this extra 25 lbs; becoming vegan; exercising more; taking l-carnitine, vitamin C, l-lysine, niacin; and modified citrus pectin, what else should I try? I’m wondering if this is why my maternal grandfather died of a heart attack at 48. I’m feeling rather anxious since I thought I had my healthy 92 yr old father’s genes. Thank you, John and everyone who shared your stories!
Hi John,
I have a theory. First my numbers: 55 year old female 5’5″ 125lbs. Active. Walk 35-40 miles a week, Swim 1.4 miles 3 times a week and do HIIT 3 times a week. Total C 186 mg/dl, HDL 75, Trig 48, LDL C 97, Ratio chol/hdlc 2.5, non HDL cholesterol 111. LDL P number is 1127 nmol/l, LDL small is 175 nmol/ (should be less than 162 for optimal), LDL Large 7126 (should be greater than 9386 for optimal, apoA 167 mg/dl which is optimal, ApoB 75 which is optimal, and then Lp(a) 197 nmol/l. So that’s the one that sucks.
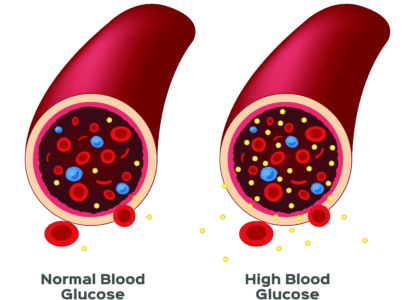
I have been Vegan for 10 years. Eat whole foods, an occasional chip of fry but no boxed foods with tons of ingredients. Eat mostly salads, veggies and lots of organic tofu, tempeh….lots of Hemp, flax, nuts, seeds, olives….avocado oil for cooking. I found out I had high Lp(a) so I went big time low carb and dropped the fruits and quinoa, rice and potatoes. I also at 55 found out I have a little insulin resistance…which is natural as we age. My blood glucose had risen so that’s another reason I went low carb. I found a great preventive care doc and he said elevated glucose causes the inflammation that the lp(a) tries to save us from. Back in the old days, people bled to death from scurvy. Some people got lucky as time went on and developed (evolved) with lp(a) that saved them from death…by stopping the bleeding and patching the cracks in the arterial vessels. People with lp(a) lived much longer than those without it. But now, we have enough vitamin C and we should be consuming more of it! If we don’t have inflammation, lp(a) won’t be needed to put bandaids on all the cracks….doing it repeatedly builds layers of plaques which lead to all sorts of bad stuff. Does that make sense? I am taking high C, lysine, proline and few other odds and ends…in a hope to prevent any more inflammation. Maybe with no inflammation the lp(a) number just sits there and does no harm?? Kind of like the STDs that hide in the body and come out and cause issues (sores) every now and then. Also I had a Calcium score done and I got a ZERO which is fantastic (and who would have thought that?) and I did a carotid ultrasound to look for soft plaques and that report I’ll get in a couple days. Anyway, Thoughts? Thanks!!
Robin,
I posted in the wrong place yesterday. I was fascinated to hear you had zero in the calcium test. Can’t wait to hear about the carotid ultrasound. I have very high Lp(a) but I also have an 88 year old mom and a 93 year old dad. I would love to get them tested. I have low inflammation markers, but my LDL is too high. Need to work on that, too. What kind of Vit C and lysine do you take? I need to find a cardiologist who understands this. I would prefer not to take statins, but I am getting scared reading all about Lp(a).
Thanks for any help.
Wow lucky you that you have your parents still!! Must be some good genes there!! I am taking l lysine and l proline plus vitamin C (just your basic kind) and Niacin — Which has shown to lower lp(a). But again the key is inflammation. Find a preventative care doctor and get genetic testing and inflammation testing done. Make sure to do an oral glucose test. See if you have any insulin resistance…it’s a normal occurrence as we age and hormones and enzymes change. If you have early insulin resistance— you can try a low carb diet…and if that alone doesn’t lower your insulin (if it’s raised) there’s a simple medicine to help lower it.
” I do not believe that mg/dl (weight) converts to nmol/L (concentration). If I am wrong, feel free to correct me in the comments.”
My chemist friend at NIH sent me this reply to the md/dl or nmol/L question.
“They are both concentrations!
mg is mass. Mole (or nmole) is used to determine relative ratios btw/ two species (stoichiometry).
“mg” is converted to “nmole” based on the molecular weight of the species in question.
If I have 100 mg sodium chloride, MW of NaCl is 58.5 mg/mmole, that is equal to 1.71 mmole NaCl.
dL = .1L
It was explained to me many decades ago why ‘dL’ is used in some applications but I forgot.
Awesome, thanks for the intel Greg, very useful.
I first ran across Lp(a) from Linus Pauling articles and confirmed it’s disastrous potential from a study I read that I believe was published in JAMA. In that study, I definitely recall levels being expressed in the 0-30+ ranges. I have to assume it was mg/dl, I don’t know what else it could be.
That study of 4000 elderly white males assessed good levels as under 22, very good levels as under 11 and very bad levels as over 30.
They participants were grouped into quintile’s The highest 20% Lp(a) group proved to have a 300% greater chance of death from all causes in the study than the lowest 20%.
I took Lysine and Vitamin C for many years thru the 90’s in quantities for 1gm each. I had my Lp(a) checked later and it was unmeasurable. I noticed zero side effects from Lysine at all, so your comment about possible side effects is very hollow in my view and especially without you having apparently tried them.
At age 63 after Hurricane Katrina I experienced what might be construed as chest pains and my cardiologist ordered a battery of tests including a stress test, thallium xray series and echocardiogram. he found nothing and most importantly he also found zero blockages.
Some years later, I had my Lp(a) measured again this time by Quest and got an apparent NMol reading which at the time I did not understand except that the amounts found were infinitesimal. I had stopped taking Lysine and Vitamin C by this time.
The article I initially read about Pauling’s experiments definitively proved Lp(a) was at the root of heart disease. In that article Pauling detailed controlled studies with guinea pigs in which he induced arterial clogging and in which he actually reversed it using Lysine and Vitamin C. Neither man nor guinea pigs produce Vitamin C internally and both suffer heart disease. Strange isn’t it? Other animals produce it internally.
His conclusion was that an inadequate amount of Vitamin C intake for collagen production to properly repair arterial damage resulted in the body using Lp(a) to patch damage instead.
The guy was hardly a “wacko” and put the finger on Lp(a) 25 years ago!
The medical community spurned him because Vitamin C and Lysine were not patent-able were they?
and there sure is a lot of money to be made treating it.
I have tried lysine for sleep, but the Linus Pauling Lp(a) protocol doesn’t have much evidence behind it for Lp(a).
I have horribly high Lp(a) so I’m really worried. I guess I need to have a cardiac CT done. I had tried Vitamin C and l-carnitine for a year but it still went up. I haven’t tried niacin. I meet with the cardiologist in a few weeks, but he seemed clueless about this when I spoke with him earlier. My triglycerides and HDL are great, but LDL is too high.
What are the side effects of Bergamot? I just don’t even know what to do at this point. I eat alot of plant foods, but have been more Paleo, so I guess I need to also cut back on meat and coconut oil (don’t have much butter already).
Help please.
Greg, can you tell me how much Vit C and Lysine you are taking? Did you start out higher and then lower the dosages as your numbers improved?
Thanks
This really has got me interested – I am 59 white female – 5’3 123 lbs, healthy and active.
LIPOPROTEIN(a) 128 NMOL/L LDL Pattern B
LDL Peak size 214.4 my 3 concerns
Chol 206, HDL 109, TRI 33, LDL 88
All my other numbers are within range – Should I be concerned and if so can I do anything?
Jacqueline, best bet is to speak to your doctor. The LDL-C is low at 88, but you’ll want to get your LDL-P number as well.
Hello i have ldl c of 123 hdl 93 and lpa a whopping 135 nmol/ i do 3 grams niacin daily as well as lysine, magnesium, methy b vitamins, pycogonel, lumbrokinease, vit c, zinc and NAC. i am planning to add 500 mg citrus bergamot as none of my numbers ever seem to budge..one issue my dr brought up and is insisting it could be a big part of my lpa numbers (not so much ldl) is i eat very clean )) but also consume what has always been thought of as heart healthy super dark chocolate, 85 percent pure, raw just cocoa beans and sugar in the bars…though stearic acid has been labeled as cholesterol neutral or beneficial there is science backing that steric acid but my LDL neutral but apparently has been shown to be the ONLY fat that raises LPA< other forms or sat fat have been show to raise LDL but lower lpa, where stearic acid, lower LDL and raise lpa your thoughts?
It’s an interesting theory to be sure, especially in light of the research linking elevated levels of sterols in the blood to heart disease.
Excellent analysis and discussion on LP(a). The links throughout to other studies and articles were also very helpful. Thank you John O’Connor!
Thanks John, very nice to hear you found the post useful!
Hi John, great post. One thing I have learned about lp(a) is that people who have high levels often have a history of premature CVD in their families (men who developed it before 50 and women who developed it before 60).
Have you looked at your family tree to see if that’s the case for you? Would also love to see another update with your numbers. My lp(a) numbers came back high — 36 mg/dL and 175 nmol/L — and I have been trying to cut back on cheese, butter and other sources of saturated fat to see how it affects my numbers. I’ve also been taking fish oil, which I’ve read can be helpful.
Thanks.
Hey Gabriella, no, I don’t have any history of early CVD anywhere in my family, but interesting suggestion. 36 mg/dl isn’t an outrageously high Lp(a) number, in fact, it’s considered in the normal range by some. How did it come on your radar?
Interesting but I take issue with a few of your points, you stated that LP (a) hides in LDl-C numbers. This is not possible. They are separate particles so I’m confused. My numbers- LDL-C 112
HDL 48
Tryglycerides 122
LDL-P 1250 ( optimal)
LP (a) 365 nmol/L (super high) so I don’t see any reason for you to worry. My LP(a) level is giving me tons of anxiety. I’m 40, diet and exercise like crazy and stuck with this genetic LPa level that is very high risk. Was started on Lipitor to lower LDL c as much as possible to mitigate effects of high LP a. Will look into niacin and deal with the side effects if doctor approves. Not sure I believe the lysine and vitamin c theory. Linus Pauling is considered a whacko for this theory. Some say aspirin regimen lowers LPa. Not sure though. Hoping they are close/working on a treatment for LPa lowering.
Jeremy,
Yes, when Lp(a) is not tested for it does hide out in the LDL-C number. Check out this study.
“The usual methods to determine LDL cholesterol do not distinguish between cholesterol derived from LDL and Lp(a) and are thus the net result of cholesterol levels from both lipoproteins. High Lp(a) concentrations therefore significantly contribute to the measured or calculated LDL cholesterol levels.”
Hi John, this is confusing. If my LDL is 110 mg/dL and my LP( a) is like 150 mg or 365 nmol how can this be?? Wouldn’t my LDL reading be higher?
Seems like the key language above is “cholesterol derived.” My reading is that there are separate cholesterol stores that are carried by Lp(a) that don’t show up unless you test for them. Would be a good question for a lab, or cardiologist.
https://twitter.com/skathire/status/902463501003870208
I think this addresses what you guys are talking about.
In what sense?
My interpretation of this graphic is that Lp(a) particles do contain apo(b) but are seperate from LDL particles, which I assume means that LDL-C and LDL-P tests would not detect at all. But I may be interpreting the graphic wrong or confused about what you and Jeremy are talking about.
The explanation for the apparent discrepancy is that an Lp(a) particle is composed of about 30% to 45% cholesterol by weight. So, in your case, with Lp(a) = 150 mg/dL only about 45 – 67.5 mg/dL are cholesterol which would bring your true LDL levels to 42.5 – 65 mg/dL
Jeremy,
have an ultrasound on your internal carotid arteries to check for plaque.
Hi Andrew. I did carotid test 2 months ago and it came out fine. I’m considering cardiac CT just to gauge how bad my calcium is. Not sure a bad outcome will change any treatments though since I’m on statin already (maybe high dose) maybe adding niacin to attempt to drop LP(a) but as I said I’m planning on pushing my cardiologist to start me on it anyway. Any other ideas?
Modified Citrus Pectin
Thanks for the great info. My Lp(a) came back very high (123 mg/dl) while the rest of my lipid numbers (LDL-C, HDL, apo-B, etc) are either low or well within normal range. I am in my mid-30s and am currently in the process of seeing if I can guage if the Lp(a) number has affected my cardiac risk in any significant way. I have a cardiac CT with calcium score scheduled in the next few months and I am trying to see if diet and supplements have any effect on my Lp(a). I find it interesting that lowering saturated fat had the effect of lowering your Lp(a) considering there are multiple studies showing the opposite.
Nate, thanks for the comment – very interesting situation. When you say your lipids are in normal range, what were the numbers? Do you know your LDL-P?
Wonder if it’s worth having your Lp(a) checked in nmol/L as well. As far as saturated fat, I don’t have direct causal proof that that was what lowered my Lp(a) number, and full disclosure I was still eating some coconut in smoothies, which is high in saturated fat, and some animal protein as well, but I saw Lp(a) drop as I cut out more and more animal products. When I finally started experimenting with a plant based diet, that was when I saw the dramatic drop to 33 mg/dl, which is 3 points out of the green in the Boston Heart diagnostics range. Of course, this is anecdotal, but I was shocked when my latest labs came back.
Thanks for the response. I really appreciate it.
My LDL-C has been around 120 over the past year, regardless of diet. My HDL-C is 40. My trigycerides went from about 75 to below 60 mg/dl when I cut down on carbs (which prior my main source of carbs were whole grains). My apo-B has been between 80-110 mg/dl and I am trying to figure out what has made it higher. I haven’t measured LDL-P directly, but I am using apo-B as a proxy.
I did have my Lp(a) checked in nmol/L which also came out very high at 269.
Over the past 4 months I have added in some carbs to my diet (mainly sweet potatoes), cut down on intermittent fasting, and increased my salmon intake from about 1-2 times per week to 4+ times per week, as well as added about 10-15 eggs a week to my diet. As I said I have a blood draw planned in the next week or so.
Otherwise my diet is what most would consider a whole food diet, with a lot of veggies (10+ servings a day), chicken about 2 times per week salmon 4 times per week, and beef a few times per month. I do eat a fair amount of ghee and grass fed butter, as well as cook with avocado oil, and use a good amount of olive oil for salad dressing. You spoke of Niacin, which I have been hesitant to take unless I know the Lp(a) is indeed causing plaque or other heart health risks. I also have some Bergamot extract supplement, which I have also been hesitant to take.
Interesting, thanks for sharing. As I mentioned in the blog, the first change I noticed making a difference in dropping my Lp(a) levels was cutting out all butter (I had also been eating a lot of grass fed butter). Lp(a) has to respond to drops in LDL-C since it’s a combo of APOA and LDL-C. For this reason, I also eat eggs very sparingly and sometimes only the whites. I realize this is sacrilege on Keto / Bulletproof type circles, but I saw a difference. In addition, you have the whole TMAO issue with eggs that I’ve recently written about here: https://www.mygenefood.com/eat-eggs-everyday-no-cholesterol-nothing/
Let us know how the next round of labs look, good to spread knowledge on this topic.
Thanks, will do.
I had one question about your diet. When you cut out butter and saturated fat, what if any oil did you use to cook with? Thanks
Hey Nate, I used oil sparingly, but focused on avoiding oxidized fats, so when I did cook with oil I primarily used avocado oil.
I also use avocado oil, but can you explain or direct me to an explanation of what exactly would constitute an oxidized fat.
I got my most recent labs back after mainly adding sweet potatoes and 10-15 eggs/week cooked in butter or ghee to an already low carb diet/whole food diet. Lp(a) increased slightly to 280 nmol/L. LDL-C increased to 137, and this is the first time I had measured LDL-P but it was higher than I would like at 1400. HDL did increase pretty substantially from 40 to 52. Triglycerides were unchanged. I have cut out the eggs and butter and plan to take your approach John for 3 months and see what the results are.
And John maybe I missed it in the post, but what was the effect of HDL over the time period you discussed?
Nate,
My HDL went to its highest its ever been at 57 mg/dl (had been 52 and 53 prior). Excited to see what happens with the plant based approach. Check back with us please.
Hi Nate,
I just found out that I have almost the same high LPa level as you mentioned. I was wondering what your calciumscore turned out to be and if you’re currently receiving any form of treatment.
Thx!