My Lp(a) is High: Here is How I Deal With It
Contents
Dear reader: the information in this post provides the basics of Lp(a) and the details of my journey after finding out their levels were elevated a few years ago. We have converted the comments section of this post to a forum where readers can share their Lp(a) stories. Discovering that you have high Lp(a) is scary and stressful, connecting with others who are in the same boat is helpful. Nothing contained in this post is medical advice. Lp(a) is a serious medical condition and requires the care of a physician. The Familial Hypercholesterolemia Foundation maintains a list of physicians who may be able to help you make sense of elevated Lp(a) numbers.
Discovering that you have elevated Lp(a) (pronounced “lipoprotein little a”) is upsetting.
I know because I’ve always had mildly elevated Lp(a).
Lp(a) production is related to inherited LPA gene variants, some of which I carry. As a result, I’ve always seen moderately elevated Lp(a) levels when I get routine blood draws.
The blog post that follows highlights some of the basics of Lp(a) research, and anticipates some of your likely questions, so you can have better conversations with your physician as you decide on a course of treatment or nutrition strategy.
First, some lipoprotein basics to set the table for the rest of the conversation.
Lp(a) under the microscope
As you can see from the chart below, the surface of LDL particles is enwrapped by a protein called apoprotein or apolipoprotein B or APOB (the gene is APOB) for short: labs and clinicians refer to it as apoB.
There is one apoB per LDL particle.
Unlike your run of the mill LDL particle, Lp(a) is a more dangerous type of apoB-containing lipoprotein. 3
Structurally Lp(a), is a cholesterol-rich, apoB-containing LDL to which a single molecule of apoprotein(a) is bound. 4
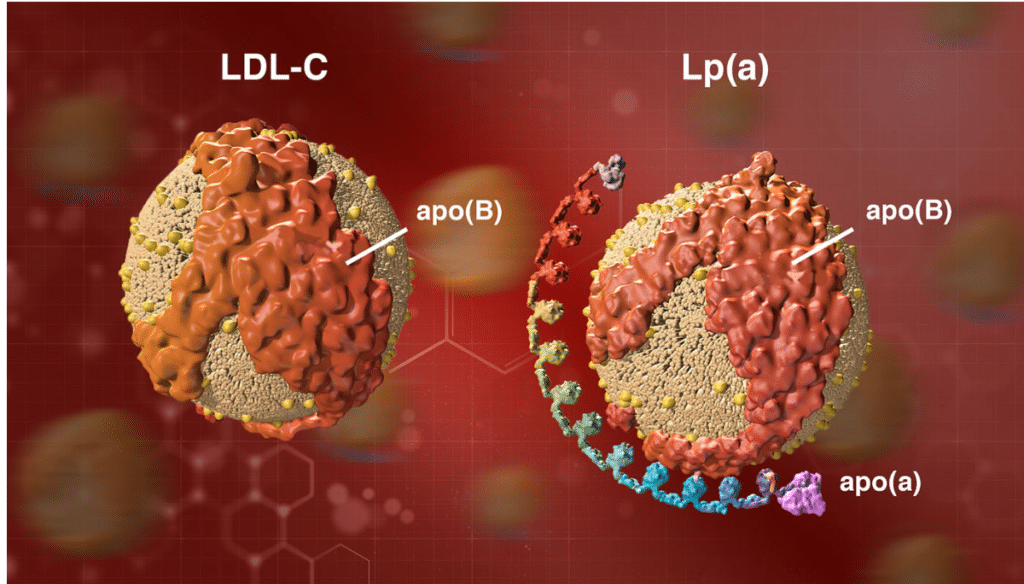
Image credit: https://www.amgenscience.com/features/10-things-to-know-about-lipoproteina/
Lp(a) testing is rare
LP(a) testing is still rare, but shouldn’t be. If you carry genetic variants that lead to high lipoprotein(a) levels, it’s important to know so you can work with a physician to treat APOB levels aggressively.
Simply doing nothing can have dire consequences.
We have seen very public examples of how elevated Lp(a) can do damage, even early in life. Celebrity trainer Bob Harper, of Biggest Loser fame, suffered a heart attack at age 52 when he appeared to be in his prime. As it turns out, the culprit was elevated Lp(a).
Although elevated levels of Lp(a) are a direct risk factor for heart disease, most “normal” lipid panels don’t even measure for Lp(a). 5
In fact, when I get Lp(a) tests done my insurance carrier often sends me a letter saying the test isn’t proven and therefore isn’t covered.
In the standard lipid panel that most of us get, Lp(a) “hides” in the LDL-C number.
What I mean here is that, absent a break out for Lp(a) specifically, Lp(a) will be included in your overall LDL-C number. 6 As the latest update in my Lp(a) numbers shows on the table below, I have had blood tests where my Lp(a) has been high despite LDL-C numbers that are fairly good at just over 100 mg/DL.
What constitutes “high” Lp(a)?
According to the National Lipid Association website, Lp(a) is considered elevated at levels greater than 50 mg/DL or 125 nmol/L.
There is strong evidence to suggest that elevated plasma Lp(a) levels (greater than 50 mg/dL or 125 nmol/L) are an independent – and possibly causal – risk factor for heart disease.
How I discovered elevated Lp(a)
Lp(a) first came on my radar after doing a Boston Heart Diagnostics Cardio panel. My lipid markers were generally ok, but at 43 mg/dl on one test, and with previous results at 46 and 49 mg/dl, my Lp(a) number was labeled “borderline.”
After reviewing my charts, my doctor told me there wasn’t much I could do to lower Lp(a).
“Lp(a) is genetic, you can’t change it all that much. It’s possible Niacin could help”
That’s never fun to hear for a metric that is tied to increased risk of heart disease, but I resolved to try nonetheless.
My Lp(a) results
While lowering Lp(a) through diet is certainly difficult, over the years, I have seen my Lp(a) number fluctuate.
Exactly why the numbers have changed is impossible to say, but I have seen rather significant changes when on different protocols.
John's Lp(a) progress
| August 2016 | |||||
| February 2017 | |||||
| November 2017 | |||||
| September 2018 | |||||
| November 2018 | |||||
| April 2019 | |||||
| June 2019 | |||||
| March 2020 |
The Cleveland Clinic references a study that looked at 5,000 patients with elevated Lp(a). When the LDL in these patients was brought down (not specified whether this was LDL-C or LDL-P), the “increased risk for mortality from Lp(a) was negligible.”
These are the studies that offer good news for those of us who need to keep an eye on Lp(a). Since Lp(a) is carried on the LDL particle, it needs LDL to do damage.
The less LDL to bind to, the less Lp(a).
This is the advice of Dr. Dayspring in the video I embedded above. High Lp(a) requires more aggressive treatment of APOB levels.
Niacin hasn’t shown real efficacy
When I first saw a blood panel that had elevated Lp(a), my doctor began discussing Niacin as a supplement, as there is some data to suggest that Niacin can reduce Lp(a) levels, although there is no evidence that Niacin reduces primary outcome clinical events in in its three major trials in persons with elevated CV-risk, and there was no event reduction even in people who saw a drop in Lp(a) when taking Niacin.
- CDP Trial – no benefit in taking Niacin
- AIM-HIGH Trial – no benefit in taking Niacin
- HPS-THRIVE Trial – no benefit in taking Niacin
The bottom line is that we have evidence that Niacin may lower Lp(a) in some individuals, but we do not have evidence it makes a difference in reducing heart attacks and strokes, and all of these trials report serious side effects in patients using Niacin.
My plan for dealing with my Lp(a)
Repatha is a PCSK9 Inhibitor that has been specifically shown to lower Lp(a) levels. I have recently switched insurance plans in favor of coverage for this drug specifically, and plan to test out my tolerance in the coming months. I would take a statin but develop bad side effects to any statin I’ve tried.
The goal here is simple, be hypervigilant about APOB levels as a risk mitigation strategy for my genetic risk with Lp(a).
Additional resources and key takeaways
For me, the key takeaway here is that elevated Lp(a) is a sign that an individual must be even more vigilant about maintaining proper “cardiovascular hygiene.” Although Lp(a) may not move with ease, it’s worth the effort to determine what drives your LDL-P number and make the changes you need to to get that number in line, which usually will mean less than 1,000.



96 Comments
Leave Comment