Breaking Down My Blood Sugar Numbers: Is an HbA1c of 5.1 Good?
Genes Mentioned
Contents
Note: This post is from a patient of mine interested in his blood sugar numbers:
This is a post about my blood sugar numbers, including HbA1c (a metric that measures average blood sugar levels over the past 3 months), why they’re relatively low and strategies we can all use to keep our blood sugar in check.
Anything below 5.7 is considered a “normal” HbA1c level by most labs.
The 3 big blood sugar tests
According to the American Diabetes Association, the big 4 blood sugar tests are: 1
- Oral glucose tolerance
- Fasting glucose
- HbA1c
When I say my HbA1c numbers are “low,” I mean they are basically in range (anything at or above 5.7 is trouble), well outside the scope of the type 2 diabetes (“T2D”) and insulin resistance. I included a chart below a chart mapping my latest insulin data.
Blood sugar basics
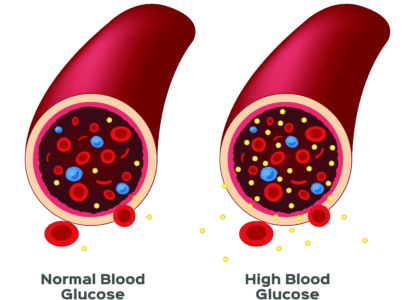
When we eat carbohydrates, the body breaks down the food into glucose, a simple sugar every cell in the body can use for energy. Insulin is the hormone the body then uses to get glucose into cells, or stored as glycogen where it is available for later use in the muscles and liver.
That’s right, since glucose is vital to life, we evolved to store it for a rainy day.
However, not all of us do such a great job of effectively using the glucose we eat.
In some cases, especially in people who are at a genetic disadvantage in clearing and using glucose, excess glucose is stored as fat, or it remains elevated in the blood which leads to a cycle of inflammation. 2
The body can only store so much glucose as glycogen. When the liver and muscles are “full” of stored glycogen, a process known as “de novo lipogenesis” allows the body to convert the excess glucose to triglycerides where we store it as fat. 3 The first layer glucose storage organs have limits on glycogen, but there is no limit to the fat that a person will store.
This is why people who have elevated blood sugar tend also to have high triglycerides, and why I included my historical triglyceride data alongside the more traditional diabetes metrics below.
What is HbA1c?
HbA1c, or hemoglobin A1c, tests measure your average blood sugar level over the past 2-3 months.
Hemoglobin is a protein found in red blood cells. Glucose in the blood “glycates,” or binds to these hemoglobin proteins. So, the more glucose in the blood, the more red blood cells bind to the blood sugar, which then gives us the ability to measure blood sugar levels over time.
The 2-3 months of blood sugar data we get from HbA1c tests correlates to the average life cycle of a red blood cell, which is about 3 months.
Why does elevated blood sugar cause inflammation?
The body wants us to use glucose, it’s central to life and universally recognized at the cellular level as fuel.
However, like everything else in the body, it has its place, and that place is inside the cell. The immune system knows this and goes on alert when glucose hangs around in the blood for too long.
When blood glucose levels stay high over long periods of time, the immune system is triggered, almost as if to say, “hey, you’re not supposed to be here, get out of here, get into the cell.” As a result of sensing an invader, the immune system releases inflammatory cytokines in a looped cycle, that over time, cause tissue damage, leading to inflammation. 4
Cytokines such as TNF-a cause damage to cells and increase levels of oxidative stress, which in turn damage fats, protein and even DNA.
Blood sugar after a meal vs. chronically high blood sugar
Blood glucose levels after a meal are called “postprandial.” New research teaches us that the postprandial blood sugar response is at least 50% genetic.
There is some evidence that the spikes in blood sugar after a meal may be an independent risk factor for certain diseases, especially heart disease. 6
This is kind of a scary proposition as most people have no idea what their post meal blood sugar data looks like. Longevity experts like Dr. Peter Attia have expressed preference for a two hour oral glucose tolerance test (OGTT) over HbA1c, presumably because of the importance of the post prandial period in driving inflammation.
As such, the idea is to keep blood sugar under control over the course of weeks and months, but also to prevent major spikes during the day.
My blood sugar numbers (HbA1c, Glucose, Insulin, and More)
| Test | |||||
|---|---|---|---|---|---|
| Insulin Resistance Score (SJC) | |||||
| Insulin, Intact, LC/MS/MS (5)(SJC) | |||||
| C-peptide, LC/MS/MS (6) (SJC) |
Ok, so let’s do a quick walk through of each metric. Of course, we have already covered HbA1c, so we will leave that out.
HOMA-IR – HOMA-IR, or the homeostasis model assessment-estimated insulin resistance, is a calculation clinicians use to measure insulin resistance. It is calculated by multiplying fasting plasma insulin by fasting plasma glucose, then dividing by the constant 22.5. When HOMA-IR is greater than 3.80, it is thought to be evidence of insulin resistance.
Glucose – How much glucose remains in the blood after going without food for at least 8 hours? Levels of between 70 and 100 mg/dl are considered normal, 100-125 mg/dl are believed to evidence of prediabetes.
Insulin – again, fairly self explanatory. This test looks at the insulin in your blood, lower is better because it signifies your body doesn’t have to work as hard to get glucose in your cells. High fasting insulin is a sign of insulin resistance.
Triglycerides – call them sugar fat or energy fat, both are basically correct. For our purposes here, it’s important to reemphasize that the body converts glucose into triglyceride fat when it has stored as much glycogen as possible for a “rainy day.” Anything below 150 mg/dl is considered normal by most labs, and my TG have been as low as 66.
Closing thoughts
In my experience, keeping blood sugar top of mind is beneficial. It blunts that voice in my head which tells me its fine to tear into a pint of ice cream or a bag of cookies. Now, of course I still get into the junk food drawer on occasion, but knowing the science of how spikes in blood sugar impact my health does help me reserve my sugar intake to the occasional treat.
As with any of the topics we touch on on the blog, the idea is not to fear glucose, but rather to learn how our bodies use it and make food choices that go with the metabolic flow, as opposed to against it.
There is a very real public health threat posed by diabetes and greater awareness of our own individual metabolic state, is I believe, a good thing.



Easier to eat low carb meals
Have you looked into R- Lipoic Acid as another supplement for lowering blood sugar? Apparently the “R” version is more potent than just Alpha Lipoic Acid.