What’s so good about ‘good’ cholesterol? Is higher HDL really better?
Genes Mentioned
Contents
A new analysis of data from the PICASSO trial has lipid lovers all a fluster.
Some folks are saying that this analysis is proof that your HDL levels don’t matter all that much. Is there any truth to that? What’s so good about ‘good’ cholesterol anyway, and is higher HDL really better?
Let’s dig in.
What does PICASSO actually say?
The PICASSO trial is the Prevention of Cardiovascular Events in Asian Patients with Ischaemic Stroke at High Risk of Cerebral Haemorrhage. There’s been lots of discussion about this trial, including this latest analysis that looked specifically at two drugs used in the trial: cilostazol and probucol, which have opposite effects on HDL-C levels. 1
The takeaway from this latest analysis of PICASSO data isn’t as wide-reaching as some commentators would have us believe. Instead, the researchers concluded that:
[P]harmacologically altered HDL-C levels may not be reliable prognostic markers for cardiovascular risk.
So, basically, if you give people with low HDL-cholesterol drugs that raise their HDL-C, this does not translate to a decrease in the risk of heart attacks, stroke, and other cardiovascular problems.
What this analysis of PICASSO data doesn’t say is that there’s no link between HDL levels and cardiovascular risk.
Why does this matter?
Well, because if you end up thinking that HDL doesn’t matter, you might totally dismiss lab results that show very low HDL.
Why should you care about low HDL levels?
In short, low levels of HDL are associated with an increased risk of atherosclerosis and cardiovascular disease. This means a greater risk of stroke, heart attack, and death.
Many well-regarded studies have consistently found that people with the highest HDL levels had the lowest risk of developing heart disease. ”2” These studies include the Framingham Heart Study (FHS), Lipid Research Clinics Prevalence Mortality Follow-up Study (LRCF) and Coronary Primary Prevention Trial (CPPT), and Multiple Risk Factor Intervention Trial (MRFIT). The CPPT and MRFIT were both randomized trials in middle-age high-risk men.
In the FHS, CPPT, and MRFIT, a 1 mg/dl increase in HDL-cholesterol was associated with a 2% decrease in the risk of heart disease in men.
The FHS also noted a 3% decreased risk of heart disease in women with every 1 mg/dL increase in HDL-C.
Similarly, in the LRCF, a 1 mg/dl increase in HDL-C was associated with a decrease of 3.7% for men and 4.7% for women in the likelihood of death from cardiovascular disease.
How does HDL support heart health?
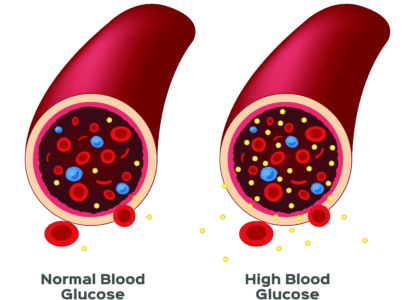
HDL’s benefits for cardiovascular health are mainly related to its role in reverse cholesterol transport. HDL helps scoop up cholesterol from the blood and carry it back to the liver for biliary excretion. This isn’t the only role for HDL, however. Indeed, there are many different types of HDL, varying in their major apolipoprotein components, density, and mobility, and these have different properties and functions in the body.
HDL may inhibit endothelial inflammation, for example, meaning it can help keep the walls of your arteries healthier. It may even promote the production of nitric oxide (NO) by the endothelium (the inner wall of arteries) as well as prostacyclin production. This would help keep arteries flexible and responsive, meaning better blood pressure regulation. HDL may also help the body to deal with potentially damaging amyloidogenic proteins, oxidized lipids, and lipids created by pathogens. ”3”
If HDL is so great, why didn’t PICASSO show that?
Turning back to the PICASSO trial, let’s consider this new analysis of trial data. In this analysis, the researchers looked specifically at whether a person’s risk of cardiovascular events changed in response to drug-induced changes in HDL-C levels. They concluded that drug-induced changes in HDL-C did not reliably predict such events.
It’s true that cilostazol and probucol led to significant (and opposite) effects on HDL-C levels during the study. However, these changes had no significant effect on cardiovascular risk. This reaffirms the disappointing failures of recent CETP inhibitor trials. CETP (cholesteryl ester transfer protein) inhibitors are drugs that increase HDL-C levels.
So, what’s going on here? Why didn’t raising or lowering HDL-C with drugs make any difference to cardiovascular risk?
One explanation is that CETP inhibitors like cilostazol don’t just increase HDL-C, they also increase atherogenic apoproteins ”4”. Conversely, probucol increases CETP and lowers both HDL-C and LDL-C levels.
Up or down, then, the change in HDL-C seen with these drugs doesn’t seem to make much difference to cardiovascular risk. That doesn’t mean that these drugs aren’t helpful, it’s just that their clinical benefit isn’t due to their effect on HDL-C. Indeed, one takeaway might be that probucol’s HDL-C-lowering effect isn’t necessarily a bad thing, and that it shouldn’t lead us to ditch the drug entirely.
Let’s quickly look at some other studies. In two large clinical trials, the CETP inhibitors torcetrapib and dalcetrapib were given to people with high cardiovascular risk. These drugs increased HDL-C levels by more than 70-100%, but this didn’t translate to a reduced risk of another cardiovascular event ”5” ”6”. In another trial, anacetrapib reduced major coronary events, but this couldn’t be attributed just to the drug’s effects on HDL-C as anacetrapib also significantly lowered LDL-C. ”7”
When might HDL be a useful marker?
Given the findings of the clinical trials just mentioned, and results of previous epidemiological research, maybe we should reframe how we think about HDL as a marker for cardiovascular risk. Instead of simply assuming that more HDL is better, regardless of how it is achieved (i.e. through drugs or lifestyle and dietary changes), perhaps we are better served by limiting the protective effect of HDL-C to healthy individuals.
Better yet, let’s get even more nuanced and consider that levels of HDL-C aren’t the same as the functional capacity of HDL-C. And, while we’re at it, we would be smart to consider that HDL-C levels aren’t interchangeable with cholesterol efflux capacity, which is the thing that really determines our cardiovascular risk.
Functional HDL and cholesterol efflux capacity
It’s worth noting that some studies have failed to find a strong link between low HDL and a higher risk of cardiovascular disease. Why? The reason may be because HDL can become dysfunctional, meaning that the activity of the HDL you have might matter more than how much HDL you have.
What affects HDL’s protective properties? In short, inflammation and diabetes. When levels of inflammation are high, oxidative processes affect apolipoprotein-a1. This is the lipoprotein that forms packages of HDL to allow it to bind to cell receptors and scavenge for ‘bad’ cholesterol. Changes in HDL can also bring about pro-inflammatory activity. The result of these changes is that HDL loses its protective effects on the endothelium (artery walls). ”8”
Basically, ‘good’ cholesterol is only good if it can actually pull bad cholesterol out of your artery walls (cholesterol efflux) and take it to the liver for processing. Cholesterol efflux is the first step in reverse cholesterol transport (RCT) and requires a cholesterol acceptor such as HDL. So, if you have low levels of functional HDL, your cholesterol efflux capacity is also lower.
The ideal TG:HDL ratio
In a nutshell, the closer your TG:HDL ratio is to 1.00 (or lower), the better. Higher than 3.00 and you’re at considerably greater risk of heart disease. In one recent study, a TG:HDL-C ratio above 4.00 was deemed the most powerful predictor of coronary artery disease. ”9”
In very healthy, trained athletes, without underlying genetic issues, TGs may be as low as 50 mg/dL while HDL could be 80 mg/dL or more, giving a ratio of 0.625. Ideally, your HDL should be 60 mg/dL or above. Anything lower than 40 mg/dL is considered low for men. For women, anything below 50 mg/dL is considered low. ”10”
These guidelines are, as always, geared towards the general population. Studies have noted that Asian Americans tend to have lower HLD-C levels than white folks and are more likely to have high TGs.
Hispanic/Latino women also tend to have low HDL-C compared Hispanic/Latino men, while African Americans tend to have higher HDL-C and lower TGs compared to non-Hispanic whites or Mexican Americans. ”10”
How to improve your HDL:TG ratio
Exercise is one of the best things you can do to improve your HDL:TG ratio. Physical activity helps use up fat stores (thereby lowering TGs) and boosts ‘good’ cholesterol. Here are some other ways to increase your HDL levels:
- Quit smoking
- Lose any excess weight
- Check your thyroid hormone levels (low thyroid function can impact HDL levels).
- Eat a Mediterranean type diet (depending on your genotype)
- Up your fiber intake.
Eating more high fiber fruits, nuts, legumes, pulses, and veggies can boost HDL. If you love juicing, switch to smoothies. That way, you’re getting all the fiber and not just the fructose.
Mediterranean diet products and other natural health products have also gained attention recently as a way to increase HDL levels. One systematic review looked at almost 60 years of research (from 1958 to 2016) and concluded that “dietary supplementation with red yeast rice, bergamot, artichoke, and virgin olive oil has promising effects on the increase of HDL-C serum levels.”
Artichoke leaf extract and virgin olive oil were especially promising; bergamot required more investigation; and red yeast rice was only beneficial for individuals who had previously had a heart attack. ”11”
The takeaway – Is it worth getting your HDL and TGs tested?
Not all blood lipid panels are the same, and you don’t always need to test for every type of lipid. Basic testing usually includes total cholesterol, LDL-cholesterol, and HDL-cholesterol. More robust tests tend to include triglycerides, apolipoprotein, particle count, and other markers. These offer a far clearer picture of what’s going on inside your body and your overall risk for cardiovascular concerns.
This latest analysis of data from the PICASSO trial highlights something that, arguably, we already knew: cardiovascular risk is multifactorial and complicated. It’s just plain foolish to focus on HDL levels alone as the be all and end all of cardiovascular risk. Sure, it’s good to know if your HDL levels are extremely low, but a moderate to high HDL level doesn’t really tell you all that much, especially if artificially raised by drug interventions. Instead, it might be far more helpful to look at your levels of LDL and triglycerides.
Thankfully, this current tete a tete in the lipidology world is largely academic. Why? Because healthy dietary and lifestyle changes that can increase HDL and HDL function also tend to lower LDL and TGs.