Why Some People Thrive on High Protein Diets (And Why Some Get Sick)
Genes Mentioned

Contents
How much protein is too much?
It depends on who you ask, on how much you train, and also on your age.
I’ve heard Dr. Peter Attia say to only eat as much protein as you need to maintain muscle mass (although his views are evolving).
Then, there are some researchers, T. Colin Campbell and Valter Longo being perhaps the most notable, that claim no one does well on a high protein diet, especially when the diet is high in animal proteins.
T. Colin Campbell, author of the China Study, bases his anti-protein stance on his work studying disease in China as well as his clinical research, especially in rat models. He proved that he could turn off cancer in rats that had been exposed to aflatoxin by feeding them 5% protein in the form of casein, and turn it back on by bumping protein up to 20% of their diets. 1
Valter Longo’s work studying longevity jives with Dr. Campbell’s. Longo’s interest is in how certain amino acids, especially those highest in animal foods like the BCAAs, stimulate the body’s cancer pathways by triggering mTOR. 2
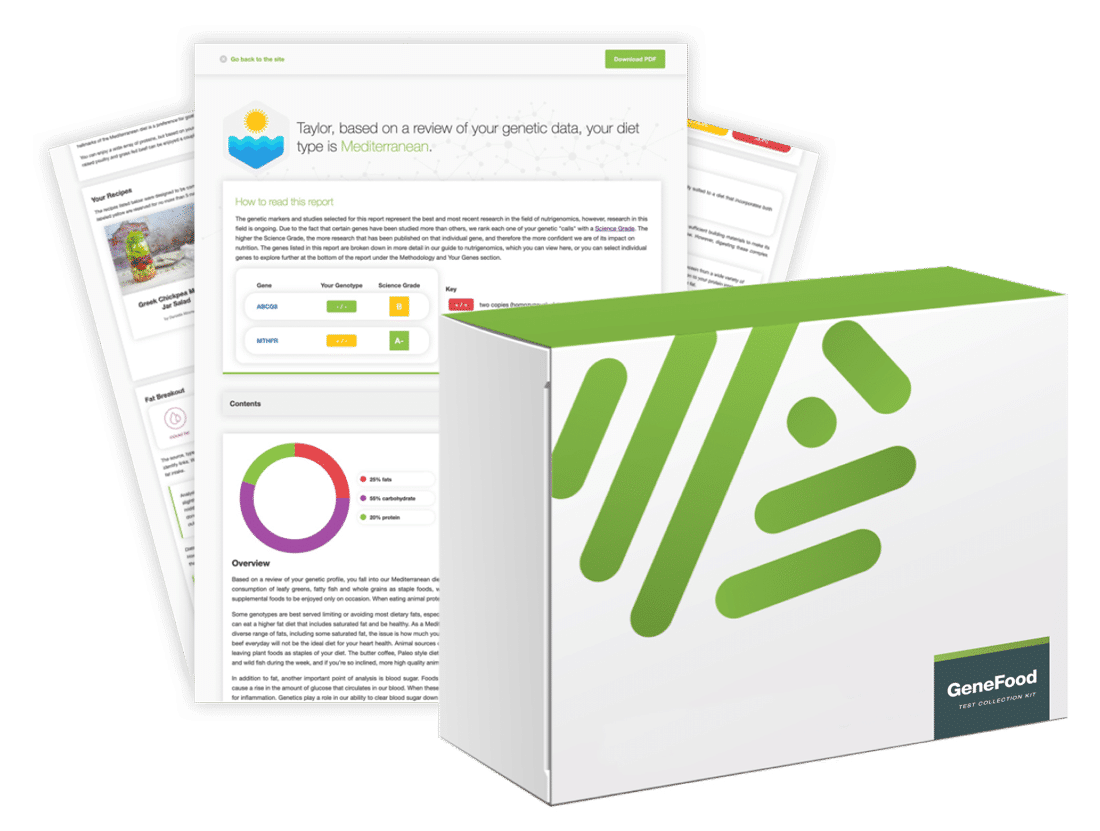
Get Started With Personalized Nutrition
Gene Food uses a proprietary algorithm to divide people into one of twenty diet types based on genetics. We score for cholesterol and sterol hyperabsorption, MTHFR status, histamine clearance, carbohydrate tolerance, and more. Where do you fit?
While Longo recommends more protein after age 65, both Campbell and Longo are low protein advocates regardless of genes. However, as we are about to learn, how your body handles protein is driven, in part, by genetics.
Genetics of protein metabolism
For example, the human body breaks down the nitrogen molecules found in protein into ammonia, and finally to urea, which is then cleared by the liver and kidneys.
Your body’s ability to process and clear this ammonia/urea cocktail is a large driver of how much protein your body can handle.
Enter the urea cycle, the process our bodies use to break down ammonia in the liver and turn it into urea, which is then excreted in urine.
When the urea cycle is functioning at 100%, large amounts of protein are easier to handle, at least in theory.
The first step in the urea cycle is governed by the CPS1 gene. CPS1 stands for carbamoyl phosphate synthase. When the urea cycle is compromised, like it can be with diminished CPS1 function, we might not do as good of a job dealing with protein waste products, like ammonia.
To quote the National Urea Cycle Disorders Foundation:
Normally, the urea is transferred into the urine and removed from the body. In urea cycle disorders, the nitrogen accumulates in the form of ammonia, a highly toxic substance, resulting in hyperammonemia (elevated blood ammonia). Ammonia then reaches the brain through the blood, where it can cause irreversible brain damage, coma and/or death.
Differences in urea cycle function explain why some seem to thrive on a high protein diet and others fall ill.
CPS1 deficiency and hyperammonemia
On one side of the spectrum are children born with severe CPS1 deficiency, who rapidly develop hyperammonemia and become very ill when they eat any protein. 3
However, the disorder is very rare.
My interest for this post is: what happens when CPS1 activity is functional, but reduced due to diminished enzyme activity?
For example, what happens if someone has just 50% CPS1 function?
Are ammonia levels elevated in these people? How do these increased ammonia levels impact physical and mental health? Does a high protein diet, which by definition means a high ammonia diet, create a toxic load the body can’t handle?
Protein metabolism varies by individual
This Harvard article does a good job framing the issue. In essence the idea is that what constitutes the “toxic” dose of protein varies from individual to individual based on how efficient their urea cycle is (and I would extend beyond the urea cycle to other areas that impact ammonia levels).
Urea cycle disorders are viewed as rare and primarily pediatric conditions, but there might be a whole range of unrecognized, genetically determined problems with protein metabolism experienced by adults. Some people may have mild mutations that compromise a gene’s function and cause slight symptoms. This may explain why one person eschews meat while another loves nothing more than a steak meal. Defects in protein metabolism may also explain why some people have bad reactions to high-protein diets like the Atkins diet.
Key takeaways
In this post, I wanted to highlight the fact that eating and digesting protein carries with it a toxic burden all its own – namely ammonia.
So how much protein should we eat?
That’s an impossible question to answer as the answer inevitably varies from individual to individual.
Many commentators recommend low animal protein diets because research indicates that, at least in high doses, certain amino acids are pro-inflammatory and can turn on cancer pathways.
Having said that, there is no consensus.
T. Colin Campbell would tell you to be vegan all your life.
Valter Longo would say mostly plants, plus fish, then bump up protein consumption after age 65 to maintain strength.
Peter Attia would probably tell you to go away, but pressed, would likely say eat only as much protein as you need to maintain muscle mass.
Still not sure whether you’re eating too much protein?
Check out our related blog post – 4 Lab Tests Every Meat Eater Should Have Done




Hello!
I’m homozygous for CBS A360A and MTHFR A1298C. In Nutrahacker report they warning me about possible high ammonia and high taurine, but I was a bit skeptical with this until I check serum ammonia and was up the roof.
– VIT D3 24,72 ng/mL
– FOLATE 4,20 ng/mL (V.N. 2.34 a 17.56)
– B-12 1053,00 pg/mL (V.N. 187 – 883)
– AMMONIA 125,11 umol/L (V.N. 11.2 a 35.4)
– HOMOCYSTEINE 8,03 umol/L
Now I low my protein intake for about 50 grams of protein per day and taking a lot of vegetables. Also I’m taking sodium phenylbutyrate, arginine and ornithine. In a couple of months I will check again my ammonia levels, I hope a good change in serum levels.
Are you on crack? Eating more than 3.5 ounces of meat per day is “high-protein”, “meathead” status? LOL! Sounds like something someone who is “flirting with a vegan diet lately” would say. Why not say something credible like, “Eating more than a pound of meat per day is high-protein, meathead status?”
I am homozygous for the CBS A360A gene as well as DAO, BHMT -08, FUT 2. I have hashimotos thyroiditis, I produce too much ammonia and cannot take Omega fatty acids. I also have trouble eating nightshades, grains and legumes unless soaked and cooked well. Cruciferous vegetable in large doses makes me very ill. Just wanted to add this because the gene is not mentioned but a very real problem for me.
Hi
I am vegetarian but I want to eat egg as a protein source bt whenever I eat egg I M facing gasetic problem very badly do me suggestion